The Gist
Medical claims process automation is capable of streamlining this time-consuming piece of the revenue cycle. But what does the right automation look like?
The medical claims process is complex and time-consuming, yet essential to healthcare as a whole. Without it, providers wouldn't get paid, health insurance companies wouldn't get paid, and patients wouldn't get accurate bills. Fortunately, effective medical claims process automation can transform this time-consuming piece of the healthcare revenue cycle and save your organization precious time. Unfortunately, many RCM automation solutions are ineffective when it comes to medical claims processing -- the end result of using robotic process automation (RPA) and other dated forms of technology. This leads to broken workflows, lost productivity, and additional work for your team. Despite the challenge of automating medical claims processing, the need for effective automation has never been more present:
89% of hospitals and health systems saw an increase in claims denials from 2017-19
~57% of health systems have 100+ open roles to fill in operations
Between denials skyrocketing and RCM departments struggling with staff hiring and retention, manual processing of claims isn't sustainable. So it should come as little surprise that 78% of health systems and hospitals are currently using or in the process of implementing RCM automation. With the healthcare claims process being as complex as it is, what does the right automation look like? And how does medical claims process automation hold up against other options, like outsourcing? To go beyond RPA and streamline your workflows with medical claims process automation, it's important to first identify key challenges in this area and potential solutions. Only then, can you begin to find the right automation and deploy your team in more effective ways.
Streamlining the claims process requires so much more than tackling claims status or follow-up. These single pieces are critical to a smooth-functioning claims workflow, but this ultimately boils down to prioritizing your people in an efficient way. Without the right automation in place, finding time to rethink how you prioritize your people is unlikely, making automation equally important in streamlining claims in today's environment. ~ Amy Raymond, VP of Revenue Cycle Operations at AKASA
Top Healthcare Claims Processing Challenges
Medical claims processing is in-depth and complex. This not only makes it difficult for many forms of automation, but also makes it rife with challenges for your revenue cycle team. The bulk of these challenges fall into two categories, each addressable by the right automation, but each too complex for most solutions available in the market.
Achieving and maintaining high clean claim and first-pass payment rates
Claims submissions that are free of errors and expected to be ready for processing and payment are known as clean claims. Clean claims are often viewed as a top key metric by hospitals and health systems. In fact, roughly 78% of such organizations measure the difference between clean claims and initial denial rates to forecast performance. Clean claims are ideal but not always easy to pull off. People make mistakes, from misentering a piece of patient info to running outdated insurance information. Any of these mistakes can dash your hopes of a clean claim and delay the entire claims process. And even if a clean claim is sent, your team is still left checking the status, which takes 8 minutes on average. Multiply that by all the claims your organization processes. That's a lot of inefficiencies. Read why AKASA experts advocate for tracking first-pass claims payment.
How automation can help
The right automation can streamline claims and reduce the likelihood of human error. For example, our Comprehensive Claim Status solution is capable of pulling and entering patient info into the corresponding field or portal. If the source information is accurate, the entry is accurate -- automation isn't prone to typos. Because Comprehensive Claim Status runs on AI and ML with support from our in-house RCM experts, it's capable of adapting to any kind of change. If a payer updates their portal or your own internal forms or fields move, the automation can adapt and continue reducing your chances of unclean claims. But the wrong kind of automation, like solutions not powered by AI and ML, will struggle with even this task. This is especially true if a field is changed or moved on a portal, in which case typical RPA bots will fail to enter the information and halt completely. That results in wasted time and money fixing the bot.
When people log into a portal to tackle a claim or update information, it's easy for us to notice a field that moved or a background color that changed. Half the time, our brains may not even notice that something has changed. We simply find where we need to go and continue working. For an RPA-only solution, that same minor change can result in the workflow grinding to a halt. ~ Amy Raymond, VP of Revenue Cycle Operations at AKASA
Optimizing workflows and realizing better utilization of employee time
Every healthcare leader wants a more efficient claims workflow, especially in this current climate of staffing challenges and rising queues. A more optimal workflow makes it possible to leave less money on the table, deliver a better patient experience, and use employee time as wisely as possible. But a number of factors make an optimal claims processing workflow difficult to achieve. Changes to payer requirements, updates to billing codes, imperfect collection of patient information, and other factors all contribute to a complicated claims processing environment. Further complicating claims, some commonly used tools can add to the complexity, rather than simplify things. For example, RPA is commonly used to support claims management workflows but can often be ill-suited for this task. RPA bots don't continue to function as intended when codes change, or an interface or webpage is updated. Human intervention (often with a high price tag) is needed to correct and update the RPA bot to address these administrative tasks. And, in the meantime, the tasks the bots are supposed to perform aren't getting worked on. With the need to use dozens or even hundreds of RPA bots to effectively support claims processing, this approach ultimately requires a significant investment of time, whether directly from staff or on the part of a consultant or service provider.
How automation can help
It's not all doom and gloom. Automation using robust AI and ML has the power to work around common issues. As previously mentioned, our Comprehensive Claim Status uses AI and ML, allowing it to adapt on the fly. The very change that makes claims workflows difficult to streamline, is the very thing that makes our automation thrive. Every new challenge -- updated rule, billing code, form, etc. -- is an opportunity for our automation to learn and continue streamlining your medical claims process.
Comparing RCM Automation Options and Alternative Approaches
The right automation, utilizing advanced technology, can streamline claims with ease. But how does automation stack up against other routes, like outsourcing? And what kinds of automation are available?
Outsourcing
Outsourcing through a third party can provide your RCM staff quick relief, allowing you to offload certain tasks and utilize your existing staff elsewhere. In some cases, it can be cheaper than hiring in-house revenue cycle people, too. But outsourcing also brings certain complications.
Outsourcing companies often utilize overseas talent, which can lead to difficulty aligning on time zones, delay communication, and make it harder to guarantee security compliance.
Outsourcers, depending on their location, can lack experience with the American healthcare system. This lack of experience can result in errors and make it difficult for outsourcers to get up to speed after any kind of payer updates or system changes.
Any time your organization updates systems or processes, you need to worry about keeping your outsourcer in the loop. This can result in costly delays.
If there's any staffing turnover or business changes with your outsourcer, you'll have to go through the onboarding process again, which can result in mistakes and/or slower processing times.
While outsourcing is appealing to many healthcare organizations, it's important to keep these downsides in mind.
Robotic Process Automation
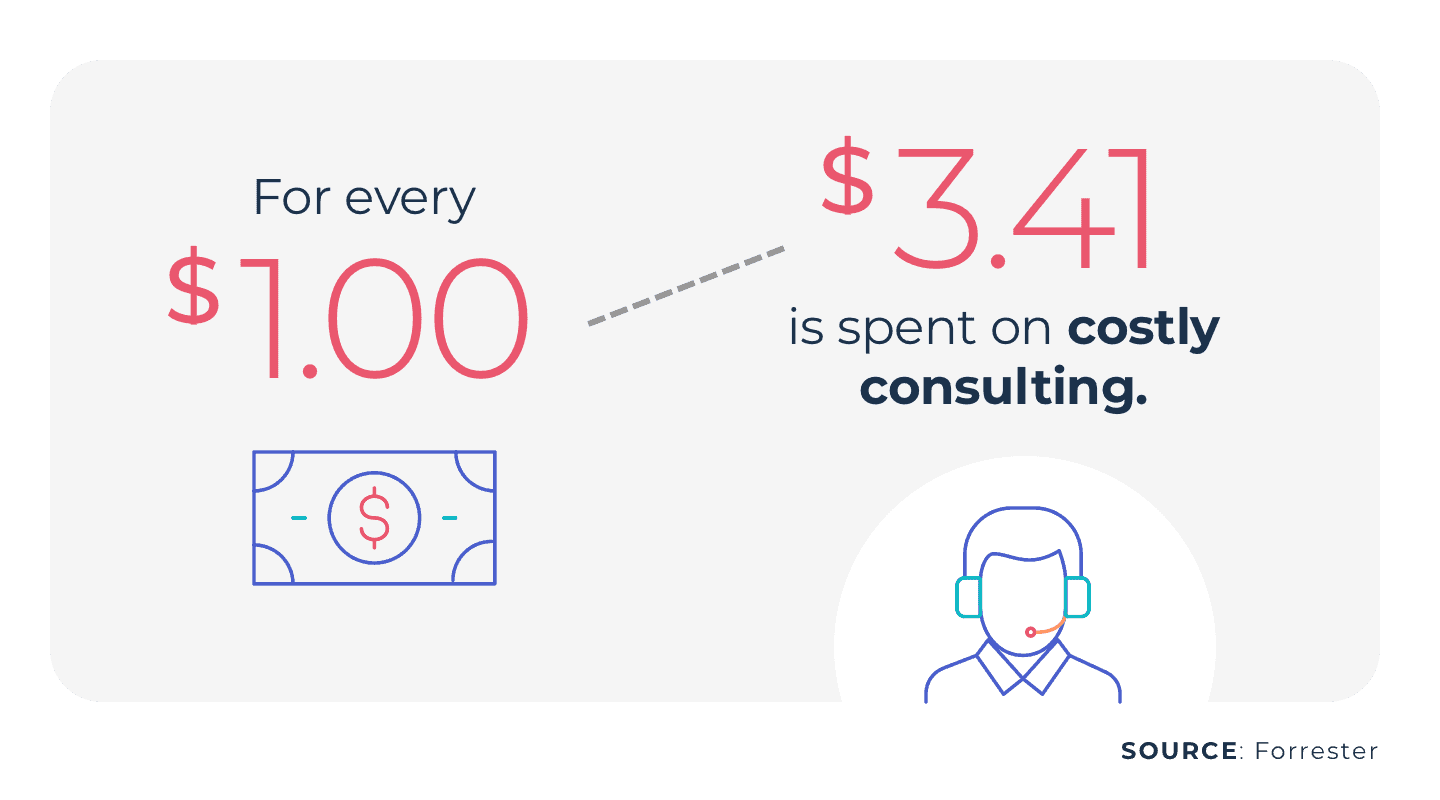
RPA is a form of automation that utilizes bots for linear, simple tasks. For linear tasks, like basic data entry, RPA can often outperform people and drive efficiency. Because RPA is better suited for linear tasks, it often struggles with medical claims process automation. Medical claims workflows are dynamic, with a number of potential challenges arising. If a payer updates a portal, your organization changes systems or moves a field, payer rules change, etc., the RPA bots will fail. Any of these single elements can break an entire workflow, leaving your organization with consulting a third party to handle maintenance or hiring an in-house specialist. Either option is costly and time-consuming, and time is something few RCM departments have.
Artificial Intelligence and Machine Learning
Unlike RPA, AI and ML -- a subset of AI -- are capable of learning as they're exposed to more data. This means they get smarter with every task they complete and every challenge they encounter. This allows automation powered by AI and ML to add value to your organization over time. This also allows these technologies to quickly learn how to handle standard claims. Even with automation powered by AI and ML, there's still the issue of handling unexpected changes or edge cases. In some cases, these advanced types of automation can figure out a new case. But in others, the change is too drastic and requires human input. This is where a human-in-the-loop approach wins. For example, at AKASA, we have a dedicated team of experts in the loop. Just like a human-in-the-loop approach, our team steps in whenever the automation encounters something it can't handle. From there, our team completes the work while the AI learns how to handle that case from there on out. The unique advantage of intelligent automation, backed by a team of experts, empowers proactive and resilient workflows that can identify and address concerns before they turn into larger problems.
What Does It Look Like To Go Beyond RPA?
There are more than 260 major RCM companies available today, with more entering the scene all the time. This makes it difficult to discern which automation vendors are capable of effectively streamlining the medical claims process, and which are going to overpromise and underdeliver. When looking for medical claims process automation that goes beyond RPA, there are several characteristics you should look for:
Specialization: The solution should be designed for the healthcare revenue cycle specifically, aligning with your needs, goals, and operational environment. Ideally, the vendor should have a background in the healthcare industry.
Adaptability: Medical claims process automation should offer value by changing, growing, and learning, leading to better claims outcomes with only limited human involvement for edge cases and outliers.
Scalability: An ideal solution should scale with your organization, as your workflows evolve and your workloads increase. It should also be capable of scaling into other RCM workflows outside claims.
Ease of implementation and upkeep: An advanced automation platform should have an easy implementation that places little burden on your team and requires little-to-no oversight or ongoing maintenance on your end -- especially when compared to fragile RPA.
Finding the right vendor goes beyond the above points. No two automation vendors are the same, and neither are any two healthcare organizations. Make sure you're fully prepared to find the right one. Discover nine things to look for when selecting your RCM automation vendor.
Go Beyond RPA With AKASA
Our automation builds on RPA with AI, ML, and a team of in-house RCM experts. We offer end-to-end RCM automation, allowing you to streamline claims and beyond. Imagine how you could more efficiently utilize your team with the following:
86% reduction in time spent on claims status checks
300+ hours of staff time saved per month
97% of claim status work queues automated
22% reduction in authorization work queue volumes
We've helped numerous health systems across the United States achieve results like those above, and we can help yours too. Go beyond RPA with medical claims process automation you can trust. See for yourself and start the conversation with our team today to see how we can help you do more with the team you have.
AKASA
Nov 3, 2021
AKASA is the preeminent provider of generative AI solutions for the healthcare revenue cycle.









