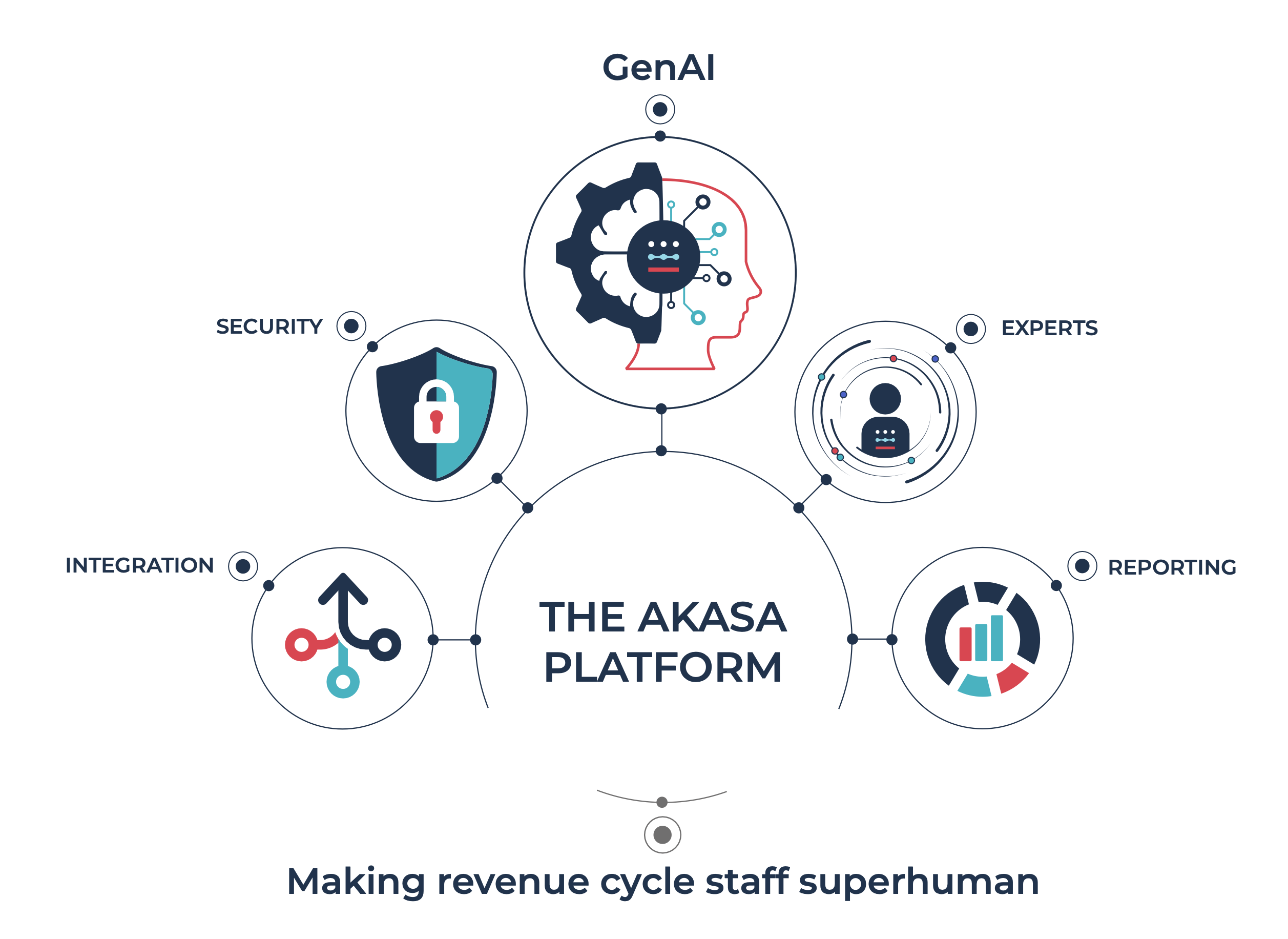
The AKASA Platform
Superpowers for your revenue cycle
Our platform integrates advanced generative AI with our deep revenue cycle expertise. By training our models on clinical data, we’re bringing you accuracy, speed, and completeness. And driving more revenue for your organization.