Jeff Francis
Vice President and CFO at Methodist Health System
Our AI simultaneously works on a batch of accounts at a time and cascades through various search options to find a matching claim. Status check results are interpreted by our machine learning or RCM experts and returned to your EHR. Accounts requiring intervention are routed to different work queues for your staff or AKASA to prioritize follow-up.
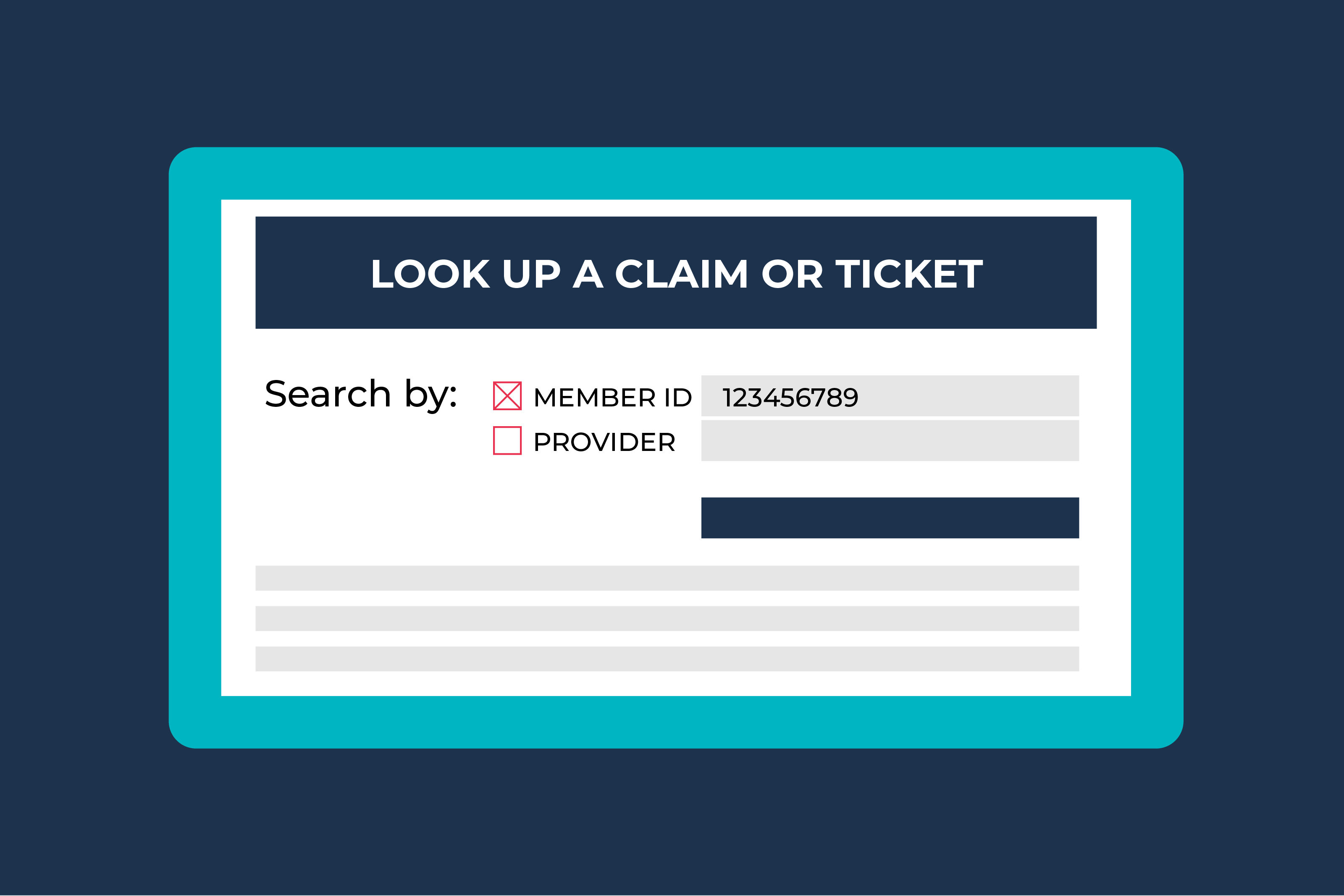
The technology determines the right time and frequency to check claim status for each payer. It simultaneously works on a batch of accounts at a time, quickly clearing your backlog. The AI continuously adapts to changing payer portals, so status checks get done — even when there are updates. It cascades through various search options to find a matching claim with a payer, ensuring high accuracy.
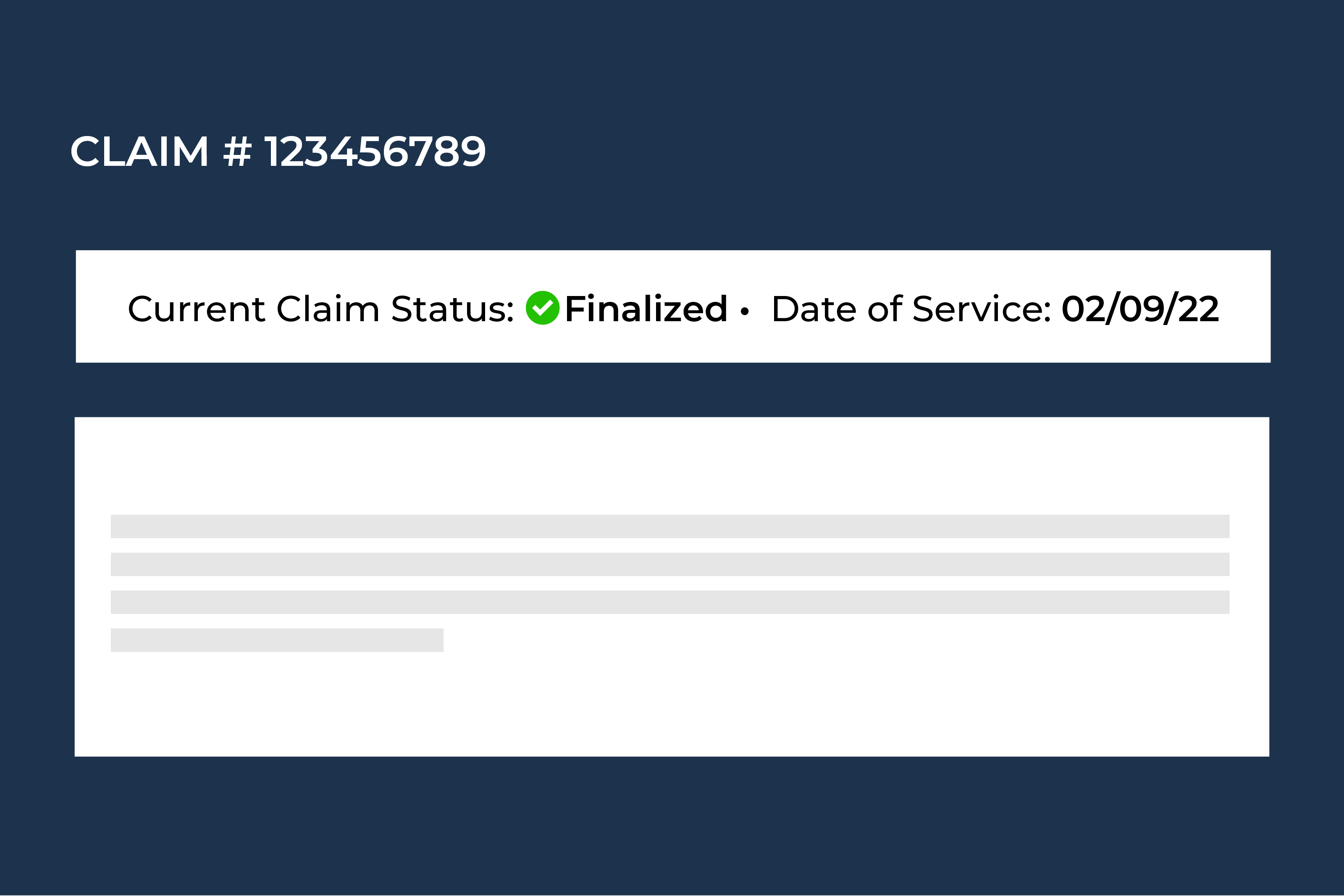
The AI obtains robust datasets, such as service line-level and payment information detail, to guide follow-up workflows. Advanced machine learning then accurately understands payer portal responses. We leverage our RCM experts to QA a subset of the claims, ensuring your results are interpreted correctly.
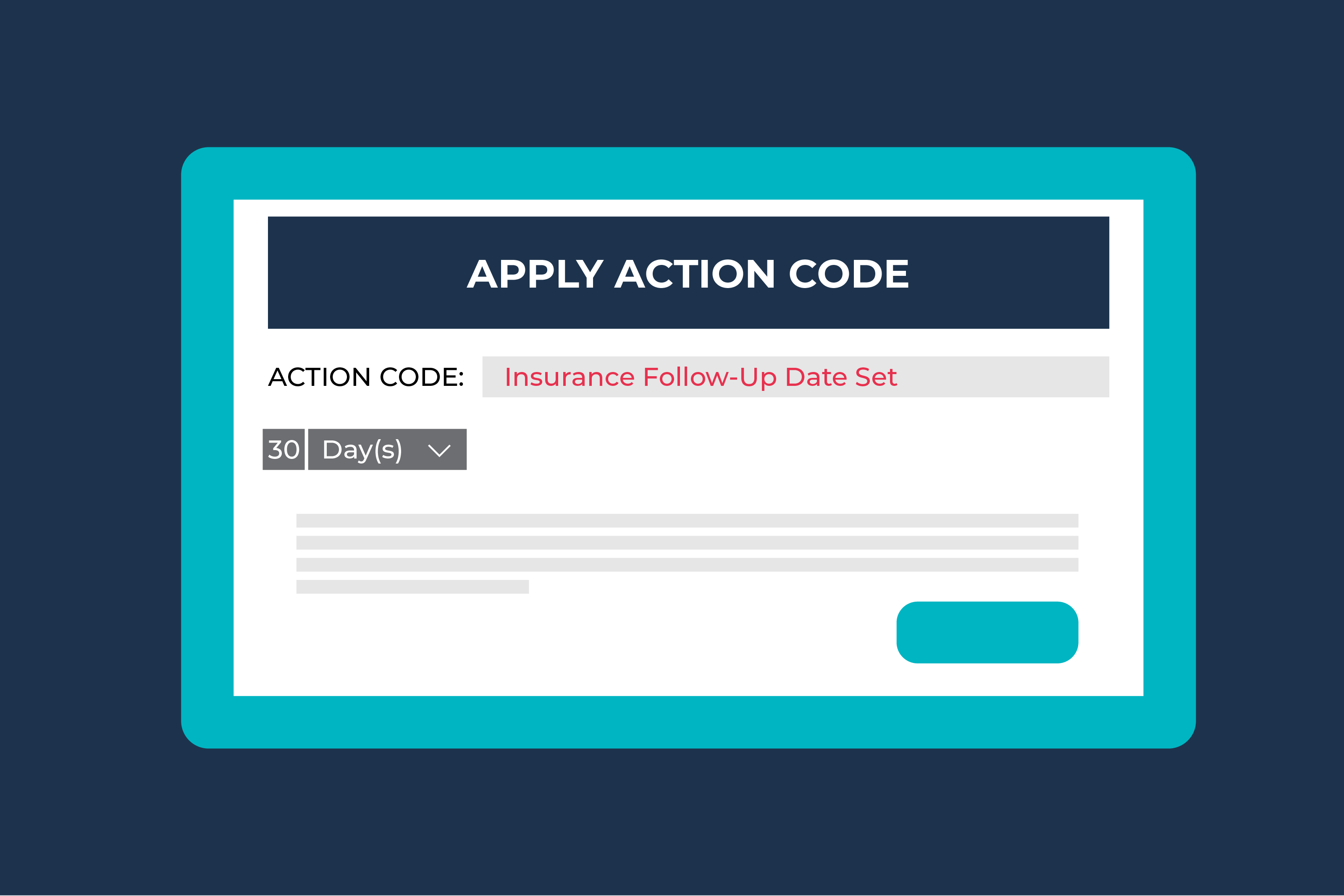
Our solution documents the status of the claim, defers it, or applies action codes based on the status. When it finds a status of no claim on file, we provide more data on why that is to help revenue cycle teams triage those claims. Our automation routes time-sensitive accounts (i.e. pending, denied, and no claim on file) to your staff or other AKASA work queues for quick follow-up. This helps your staff focus on problematic accounts, eliminating unnecessary touches.
Proactively check on the status of claims to guide follow-up efforts on time-sensitive accounts.
Quickly respond to problematic accounts to reduce A/R days and improve speed of claim resolution.
Strategically focus your team on more complex workflows. It will improve job satisfaction — and overall metrics.
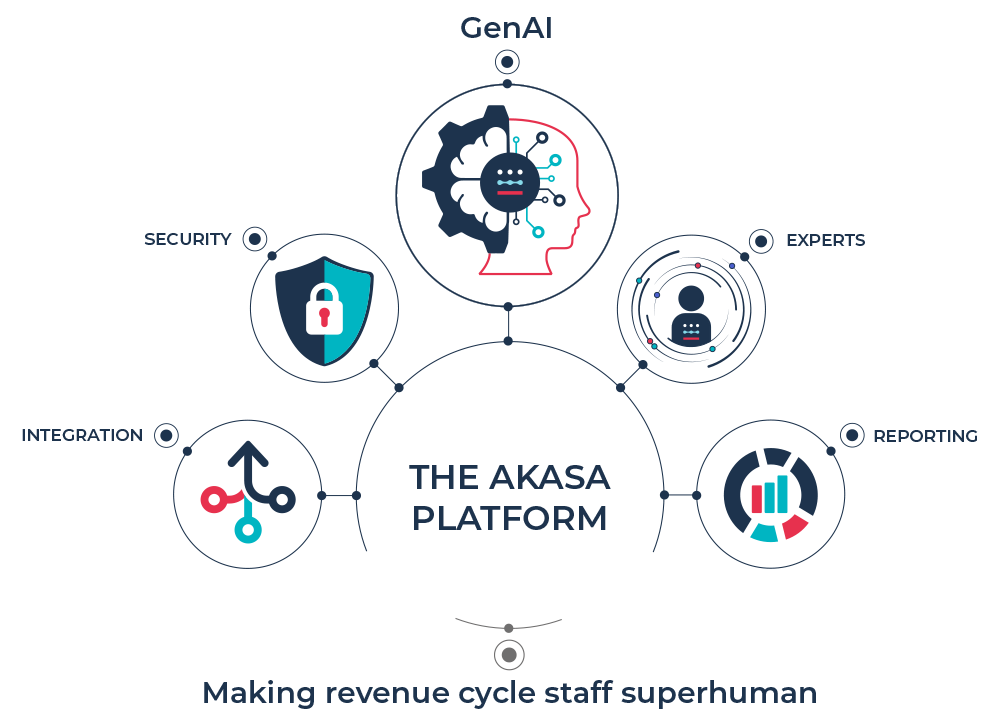
Our platform integrates advanced generative AI with our deep revenue cycle expertise. By training our models on clinical and financial data, we’re bringing you accuracy, speed, and completeness. And driving more revenue for your organization.