The Gist
Prior authorization can lead to delays and drawbacks for staff, providers, and patients. The right AI-powered healthcare RCM solution can streamline prior auth and give precious time back to staff. While prior auth is complex, with many variables and branching paths, there are three areas where AI-powered solutions can make a big difference in this time-consuming RCM process.
Prior authorization is a frequent source of frustration for many working in healthcare RCM. While deemed necessary by payers as part of the reimbursement process, prior auth is an increasingly-time consuming piece of the revenue cycle puzzle:
The average prior auth request and status check take 12 minutes and 7 seconds.
Prior authorization isn’t just a time sink, it’s also a burden — 88% of physicians associate a high or extremely high burden with prior auth. And another 79% say the prior auth process always, often, or sometimes leads to patient abandonment of care.
Making matters worse, many providers note an increase in prior auth requests for prescriptions and medical services. This increase, paired with the average time of an auth submission, means a large loss of valuable time.
Fortunately, modern AI-powered healthcare RCM solutions are capable of streamlining prior auth, allowing RCM specialists to focus on more high-value tasks and improving the patient experience.
To better illustrate the value of prior auth technology, let’s look at three prior auth processes the right AI-powered solution can take off your team’s collective plate.

1. Identifying Prior Authorization Requirements
One of the main challenges of prior authorization is meeting the ever-changing payer requirements. For some payers, requirements change a few times throughout the year, while others change their rules several times.
Whether a payer updates requirements every two months or every quarter, every prior auth requirement change can throw hundreds of new variables into the mix, complicate the auth process, and increase your chances of denials.
In the past, this was a problem with a clear solution — hire more RCM staff. Staffing challenges in the revenue cycle are commonplace today, making it difficult to hire staff to stay on top of payer requirements. There’s also the option of outsourcing payer requirements, but this brings the added complications of managing partnerships outside your organization.
Payer changes around preauthorization requirements and increased demand to schedule diagnostic procedures as soon as possible is driving significant volumes for financial clearance. Hiring to handle these volumes can be challenging and isn’t always the most strategic solution.
~ Cynde McCall, Director of Patient Access and Health Information at Methodist Health System
Solutions powered by AI are the next natural answer to this issue, but with a catch. Because payer requirements can change numerous times throughout the year, some forms of AI are either incapable or lack the flexibility to stay on top of requirements without extensive maintenance.
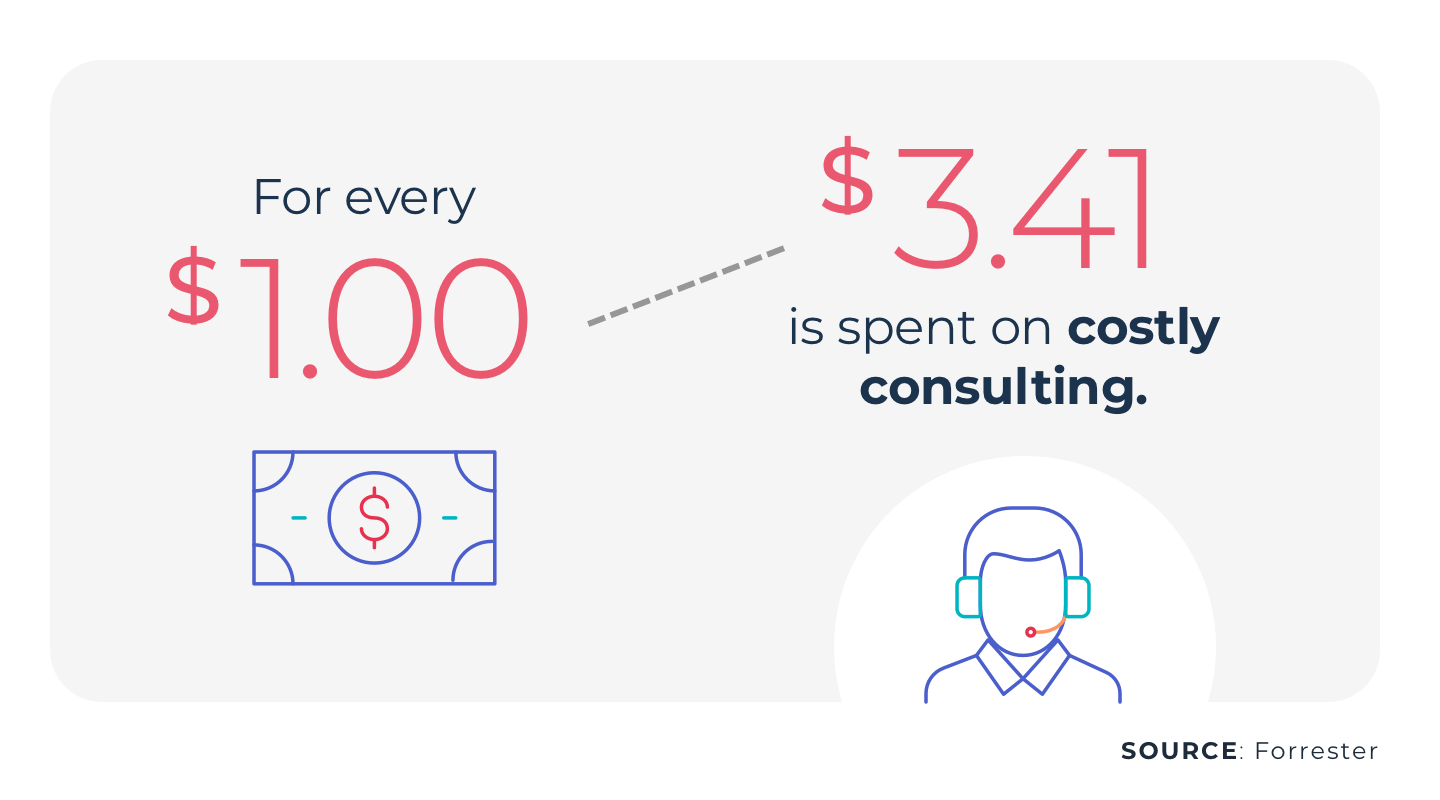
For example, let’s look at older automation technology. Many automation vendors used to deploy traditional robotic process automation (RPA) for streamlining linear tasks. RPA works well for individual pieces of larger processes, but when payer requirements update, the bot itself requires an update. Frequent updates mean costly consulting firm fees or hiring internal specialists capable of maintaining the RPA bots.
Similarly, basic forms of AI can mimic human expertise, but don’t learn as they work. Generative AI paired with large language models (LLMs) can log into a payer portal — the source of truth regarding auth requirements — to check if an auth is required before submitting the actual request. This not only saves your team the time of updating requirements, but also curbs requirement-related auth denials. And, if you’re currently outsourcing the task of updating payer requirements, this type of solution allows you to keep your operations in-house and remove the risks and complications of an outsourcer.
Read more about how AI-powered automation can address the challenges of prior authorization.
2. Submitting Authorization Requests
Ever-changing payer requirements are only one piece of the prior auth struggle. Next, it’s time to submit the authorization request.
Submitting an auth request requires checking numerous boxes and pieces of info, not to mention logging into various portals. It should come as little surprise that prior auth is time-consuming and presents numerous opportunities for errors or missing information.
Remember: it takes 12 minutes on average for someone to submit and check the status of an auth request.
Because prior auth requests are such a data-driven task, they make a great candidate for solutions powered by LLMs and GenAI. Yet, many solutions fall short here as well.
Portals often vary from payer to payer, and like auth requirements, they get updated and changed. Whenever a portal’s changed — a button is moved, field changes, a pop-up window is added, etc. — traditional AI solutions will often break and require help.
Unexpected disruptions in a prior auth solution can lead to lengthy delays, as your team may not even be aware the platform or tool hit a snag. This leaves your team stuck with manually submitting prior auth requests and playing catch up.
While many solutions are incapable of handling prior auth submission, GenAI-powered solutions are capable of navigating the complex workflows of prior auth.
For example, AKASA Authorization Management runs on GenAI and LLMs, with support from a team of dedicated revenue cycle experts. This enables the platform to first determine if prior auth is required. Once prior auth requirements are confirmed, the platform can navigate to the proper portal, log in, fill out the auth request form, answer any clinical questionnaires, and attach any necessary medical records for the request. It also includes any supplemental diagnosis and procedure codes that typically go with the reason for the visit. This helps reduce the likelihood of a retro auth, saving your team additional time and headaches.
3. Tracking Authorization Requests
Tracking authorization requests, or status checks, are a frustrating, yet necessary, piece of the prior auth process. You’ve determined auth necessity and submitted the request, only to have to manually log into the portal and check the status of the request. Meanwhile, other requests and claims and patient needs are piling up.
Prior authorization is already eating up the valuable time of revenue cycle specialists. But, few things are a greater candidate for streamlining by way of AI than auth status. Checking work you’ve already done to see if there’s an update? Imagine the other, more impactful things RCM specialists can do with that time.
~ Amy Raymond, SVP of Revenue Cycle Operations and Deployment at AKASA
With the right RCM solution, you can easily streamline authorization status checks. This allows your team to focus on complex follow-ups, improve the patient experience, and tackle tasks requiring the human touch.
Finding Time With Authorization Management
Prior authorization may only be one part of the lengthy revenue cycle process, but it’s a time-consuming part that doesn’t have to be such a burden. With the right solution, your team can narrow their focus and make a bigger impact across your revenue cycle.
The AKASA Authorization Management solution is here to help.
Authorization Management is capable of helping you resolve more prior auths, reduce turnaround times, ensure reimbursement, reduce staff frustrations, and drive timely patient care. This is all possible because of Authorization Management’s ability to:
- Determine if prior auth is required, and if so, initiate the authorization
- Check the status of submitted auth requests
- Attach required medical records and document submissions in the EHR
- Automatically include common supplemental codes during prior auth submission
- Improve as it goes, thanks to GenAI, LLMs, and a dedicated team of RCM experts
Authorization Management can work with various payer portals and requires little-to-no lift from your IT team. And best of all — it doesn’t interrupt your existing workflows.
You’ve worked hard to build the team you have. Make sure they’re working on more important tasks and making the biggest impact possible by taking prior auth off their plate.
Schedule a demo to learn more about how AKASA can help you streamline your prior auth process and better utilize your team.