Cyndi McCall
Former Director Patient Access and Health Information at Methodist Health System
We're automating the complex and time-consuming work of checking auth statuses with AI-powered automation and our revenue cycle experts. Your staff can then focus on more critical tasks.

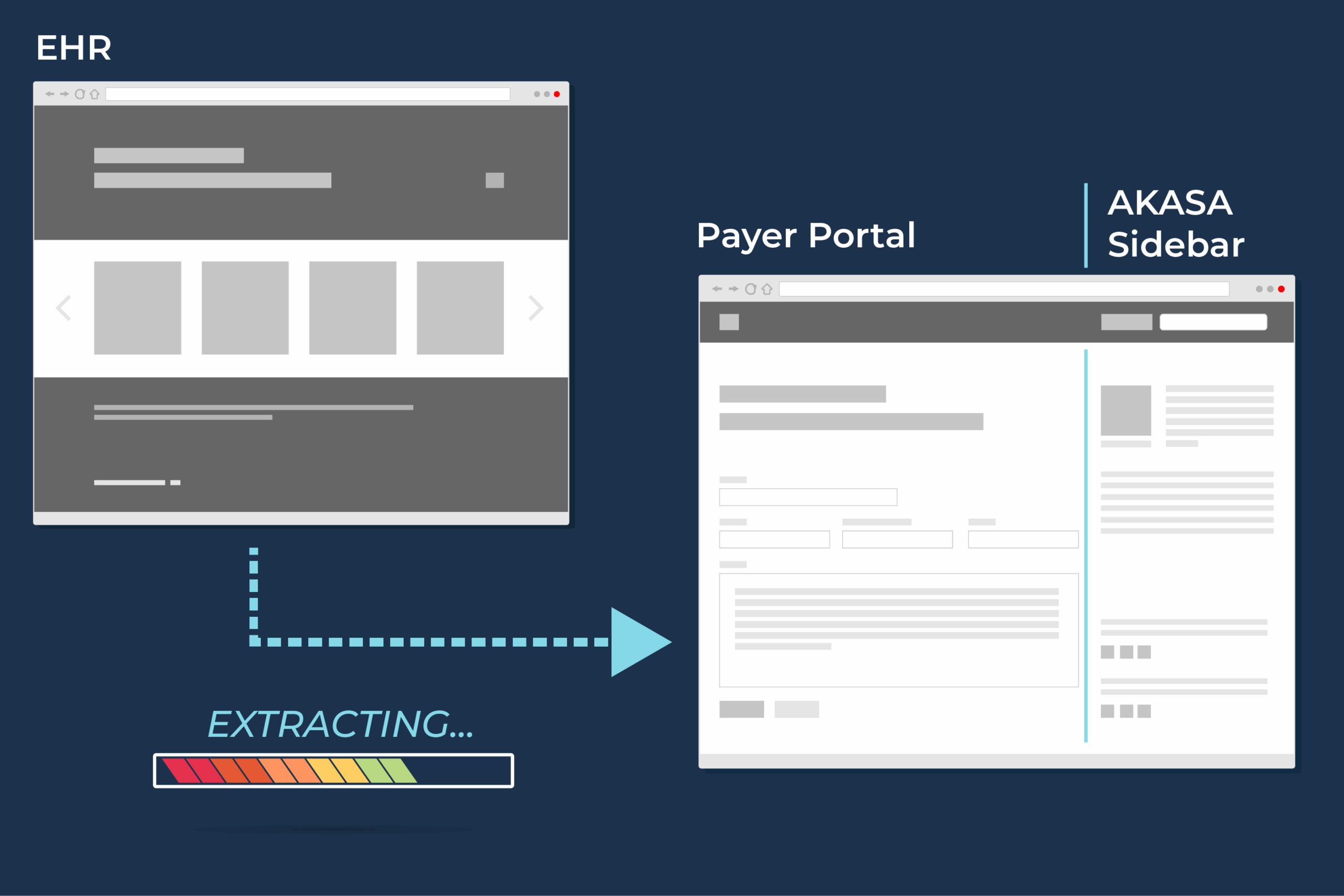
Obtains well-timed auth statuses for pending auth requests on payer portals.
Advanced machine learning accurately understands payer portal responses and leverages our RCM experts to QA a subset of the claims, ensuring your results are interpreted correctly.
Documents the auth status with approved, pending, or denied details and portal screenshots.
Free your staff from tedious and frustrating prior authorization tasks so they can focus on more complex and revenue-generating concerns.
Accelerate status retrieval by automatically checking payer portals — no more waiting or manual lookups.
Handle higher volumes of auth status checks without increasing staff workload.
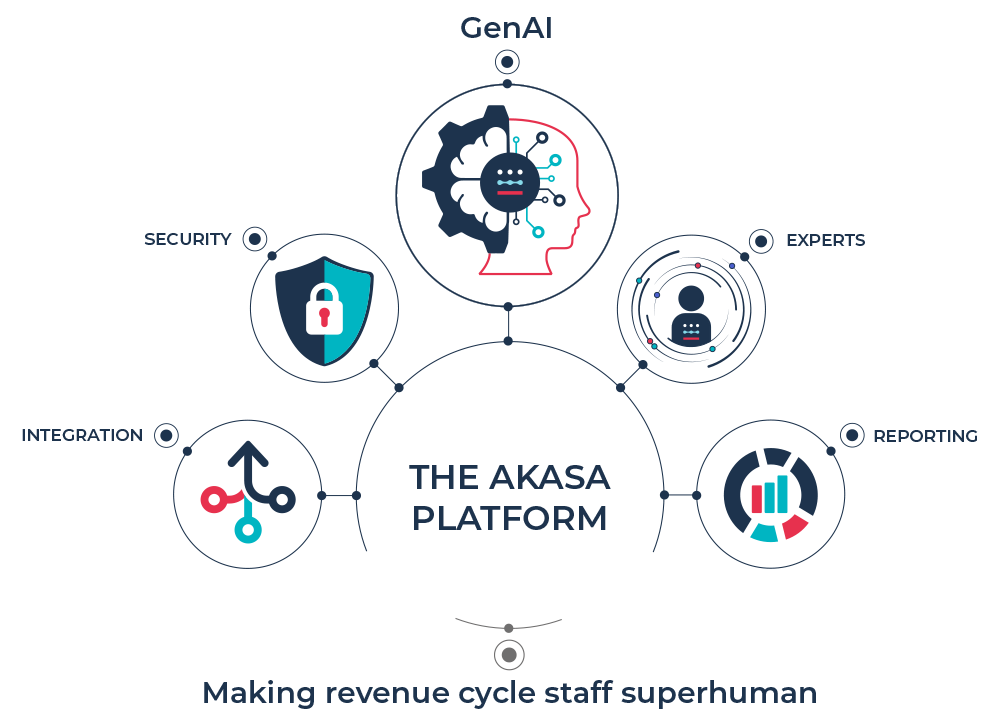
Our platform integrates advanced generative AI with our deep revenue cycle expertise. By training our models on clinical and financial data, we’re bringing you accuracy, speed, and completeness. And driving more revenue for your organization.