The Gist
Lean, a business philosophy, has been around for more than a century and was adopted by the healthcare industry in the past few decades. The idea is simple: reduce waste and provide more value. As healthcare organizations continue to look for ways to improve quality and efficiency and provide a better patient experience, lean principles can help. But only if they’re executed the right way. And revenue cycle management and lean can be a great partnership to help improve the back office. The principles behind lean and AI-powered automation go hand in hand.
Lean is a philosophy and concept that dates back to the early part of the twentieth century, with roots in the automotive industry.
Yet in the last 30 years or so, lean has been widely adopted by the healthcare industry and has become an integral way to improve quality, focus on efficiency, and reduce waste.

Nearly 70% of hospitals and health systems use lean principles for business process improvement, according to a recent AKASA survey. According to a February 2021 study in the Joint Commission Journal on Quality and Patient Safety, a higher degree of lean implementation is associated with lower adjusted inpatient expense per admission and 30-day readmission rates, an appropriate and efficient use of imaging, and higher HCAHPS scores.
The specific ways in which lean is used largely depend on the organization, its goals, services, and resources, but overall, lean is focused on standardization, continuous improvement, and adding value.
For example, hospitals and health systems that embrace lean principles often also include automation as a strategy to achieve success. According to that same AKASA survey, more than 60% of those respondents also employ automation within the revenue cycle to reduce waste and improve efficiency.
As healthcare organizations continue to innovate and identify solutions to their biggest challenges, lean will likely become even more important to their overall success.
Here, we take a look at lean in healthcare, cite use cases, discuss how revenue cycle management and lean complement each other, and offer tips for implementing lean into your organization. But first, let’s explore the origins of lean.
A History of Lean
The concept of lean originated at the beginning of the twentieth century with the automotive industry.
In 1913, Henry Ford introduced the idea of using interchangeable parts, standardization, and the world’s first assembly line for cars. Then in 1930, building on Ford’s innovation, the Toyota Production System was born. The system, which is often referred to as a “lean manufacturing system,” or a “Just-in-Time” (JIT) system, was designed to combine continuity and variety and make the production process quicker and more efficient. The Toyota Production System was developed from two concepts: “jidoka,” or “automation with a human touch,” whereby the equipment stops when there’s a problem to prevent defects; and “Just-in-Time,” or making only “what is needed, when it is needed, and in the amount needed.” Despite its rich history, however, the term “lean” wasn’t coined until 1990 in the book, “The Machine that Changed the World” by James P. Womack. Today, lean is defined as creating more value for customers with fewer resources, according to the Lean Enterprise Institute.
What is Lean Healthcare?
Two of the leading priorities facing the healthcare industry today are improving quality and reducing waste.
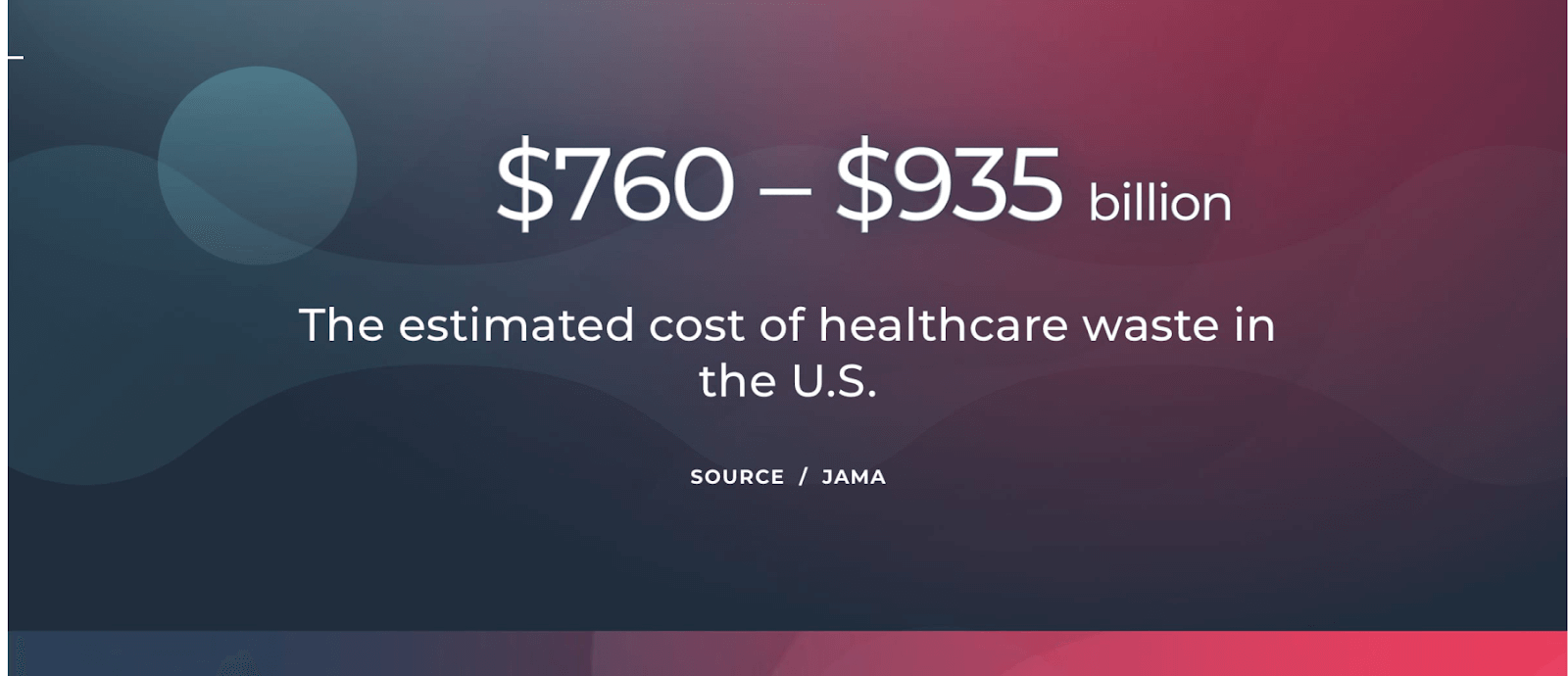
According to a 2019 study in JAMA, the estimated cost of waste in healthcare in the U.S. is between $760 billion to $935 billion, which accounts for approximately a quarter of total healthcare spending. Lean healthcare looks to address these issues and is defined as “the application of ‘lean’ ideas in healthcare facilities to minimize waste in every process, procedure, and task through an ongoing system of improvement,” according to a 2018 article in NEJM Catalyst.
The idea is to identify ways to reduce waste in the form of money, time, and supplies, reduce staff and patient burdens, and add value for patients by providing the best care and ensuring patient satisfaction.
Lean healthcare principles can also help drive engagement among healthcare workers and reduce burnout.
Although it’s not a goal of lean, one of the outcomes is often lowering overall costs — something the healthcare industry has been grappling with for years.
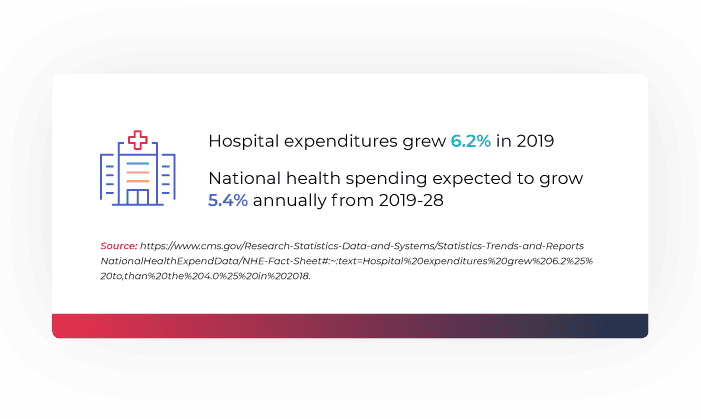
According to the Centers for Medicare & Medicaid Services (CMS), hospital expenditures grew 6.2% to $1,192.0 billion in 2019 — faster than the 4.2% growth the year before. CMS also estimates that national health spending will grow at an average annual rate of 5.4% for 2019–28, reaching $6.2 trillion by 2028.
What’s important to note, however, is that lean healthcare is about much more than saving money, according to the Virginia Mason Institute, a pioneer in lean healthcare, and creators of the Virginia Mason Production System (VMPS).
They state: “Lean organizations focus on sustaining high levels of quality, safety, satisfaction, and morale. They do this by aligning the entire workforce around a consistent management system and using that system to promote, test, and implement process improvements on an ongoing basis.”
Lean Principles in Healthcare
John S. Toussaint, MD and Leonard L. Berry, Ph.D. describe the six lean principles of healthcare in an article in Mayo Clinic Proceedings:
Lean is an attitude of continuous improvement: rather than a one-off project, lean requires ongoing management, setting higher standards with each success, and seeing failures as the momentum to move forward.
Lean is value-creating: focus on creating more value for healthcare consumers and reducing waste.
Lean is unity of purpose: united goals, objectives, and organization-wide buy-in are necessary.
Lean is respect for people who do the work: principles shouldn’t be forced, but everyone should work together, listen to each other’s ideas, and have an environment that allows for idea-sharing.
Lean is visual: visual cues and improvement software with dashboards and value stream mapping (VSM) can support lean principles.
Lean is flexible regimentation: standard work provides a starting point that can be improved. Flexibility is key, but challenges should be documented and measured against past results.
Lean Healthcare Examples
Lean principles in healthcare can be used in various ways.
For example, organizations that implement lean strategies can decrease equipment idle time, supplies and medications, and reduce costly hospital re-admissions.
Lean in healthcare can also eliminate unnecessary tests, decrease mistakes in medical records and claims, and reduce administrative redundancies.
In the early days of the COVID-19 pandemic, Hartford Healthcare implemented lean principles to reduce waste in areas like testing, supplies, and staff movement. With increased efficiencies, their clinics became the largest COVID-19 testing provider in the state and they opened up several vaccine “mega-clinics.” Earlier this year, Mount Sinai Morningside, a hospital in New York City, used lean principles to create and operationalize a COVID-19 vaccination pod. For example, each vaccination bay was equipped with standard supplies and a set-up diagram which prevented delays due to missing or excessive items and saved staff valuable time.
Revenue Cycle Management and Lean
Lean can also be used by healthcare organizations for revenue cycle management. This is especially true when it's paired with automation, as revenue cycle automation can reduce variation and increase productivity — both key tenets within lean principles.
We're seeing that for organizations actively employing lean management principles, leaders quickly recognize the value of automation within the revenue cycle and conversion to automation happens swiftly — especially for larger organizations with more overhead. ~ Amy Raymond, VP of revenue cycle operations at AKASA
Automation in revenue cycle management can expand revenue capture, accelerate cash collections, improve clean claims rates, increase first pass-payments, identify gaps to reduce denials and days in AR, and decrease the overall cost to collect.
Fundamentally, lean principles are rooted in continuous improvement and largely focus on reducing waste. Within lean, waste is identified in eight areas that should be considered and recognized while evaluating current processes and implementing new ones.
The eight areas of waste and potential RCM examples include:
Defects: Efforts caused by rework and incorrect information Ex: Working eligibility-related denials
Overproduction: Production is more than needed or being performed before it should be needed Ex: Touching each claim for review prior to sending
Waiting: Wasted time waiting for the next step in the process Ex: Employees waiting for work to be assigned
Non-utilized potential: Not using skills and knowledge of people to their full potential Ex: Employees focused on manual corrections instead of being focused on revenue generation or collection activities
Transport: Unnecessary movements or products & materials Ex: Sending work from queue to queue to complete a task
Inventory: Excess products and materials not being processed Ex: No show/canceled appointments that need to be filled
Motion: Unnecessary movements by people Ex: Tasking out work to other areas when it can be resolved in one or can be resolved upstream in the process
Extra Processing: Activities in the process that aren’t adding value Ex: Management review and approval of individual tasks after they’ve been completed
How to Implement Lean in Healthcare Revenue Cycle Management
Since every healthcare organization and revenue cycle varies in the structure, operations, and services they provide, the way in which lean principles are used will also vary.
Yet overall, lean requires that the organization focus on their patients’ needs, add value, and reduce waste. Here are some tips to consider before launching a lean initiative at your organization and for your revenue cycle department:
1. Get Buy-in at All Levels
Revenue cycle management and lean can help your organization by focusing on efficiencies. But before lean can be implemented, an organization must have a shared vision and buy-in at all levels, including the executive team, board, chief of staff, physicians, and leaders to change the culture and drive employee engagement.
Even if a project is deemed to be revenue cycle-related, process changes may involve or impact clinical or other departmental operations. Garnering this support in advance will help ensure leadership and outside departments are aligned to the goal and outcome. For example, let’s take a look at DNFB.
An increase in time to final bill could be for a variety of reasons. For example, delayed or missing charge entry, incomplete provider documentation, and claim edits are all scenarios that can contribute to inflated DNFB.
In these scenarios, a revenue cycle leader will likely have to branch out to other areas (providers, charging, coding, clinical leadership) to understand the full process today and what contributes to the increase in time to final bill. Support from executive leadership and departmental leaders will help ensure resources to complete the evaluation and implementation of lean improvements.
2. Assign a Leader
Before launching a new project, identify an internal leader who can organize teams, and encourage and motivate employees around shared goals.
This leader could be someone who leads regular revenue cycle governance meetings, or if a project is specialized, could be a specific department leader. The leader doesn’t necessarily need to be the subject matter expert but should be able to connect with those who are and take their processes and experiences to work with them to implement and measure improvement.
3. Learn About Lean
Consider hiring a consultant and get training from lean experts. The Lean Enterprise Institute and ASQ offer a host of education and training opportunities. Once leaders are well-versed in lean, provide educational and training opportunities for those at other levels as well.
4. Create Value Stream Mapping (VSM)
VSM is a lean tool that uses a flowchart to detail every step of the process. The VSM should explain both the current and future processes and include a plan and timeline for implementation.
In order for continuous improvements to be implemented successfully, it’s important to fully understand today’s process. Start with a problem and map what occurs before and after to build out the process in full. Once complete, identify areas of waste within the process. Once identified, leverage “The 5 Whys” to get to the root of why the waste is occurring.
The 5 Whys is an exercise used to understand the root cause of why a waste may occur and help brainstorm ways to reduce or eliminate the waste. Start with asking why the waste occurs and participants give reasons based on their experience. From there, branch off of those reasons by asking why again, and then repeating the process until “why” has been asked five times (or more).
Oftentimes, adjustments to the areas of waste (rather than a full overhaul of the process) can help improve revenue cycle processes.
Using the example of trying to reduce DNFB, process mapping may show that missing or incomplete documentation causes waste in the holistic process. Start the 5 Whys exercise to get to the root of why this occurs:
Why is documentation missing or incomplete?“ED providers are always late or missing documentation.”
Why?“Many ED providers are contracted and don’t finish their documentation until their next shift at our facility.”
Why?“They don’t have the same policies in place as the providers who are employed at our facility.”
Why?“It wasn’t something we negotiated with the agency.”
Why?“It wasn’t a problem we anticipated.”
This exercise can help revenue cycle teams start to understand what might be a root cause of waste and where it may make the most sense to focus on improvement.
This type of exercise can be used for any feedback on why the waste occurs. There will likely be multiple answers. Once ideas have been brainstormed and explored for how to feasibly approach, a future state process map can be created and the new process can be deployed and measured.
5. Track the Data
Data increases transparency and allows employees to look at their progress and stay accountable.
In the above example, revisiting the contracted physicians’ policy is something the RCO team may want to do. If they’re able to set this policy, they can track progress against multiple areas, such as DNFB, DNFC, time for ED providers to complete documentation, or volume of encounters that exceed the time allowed for documentation per policy.
6. Build on Early Wins
Once the first lean project is complete and everyone can see the results, use the excitement to launch more projects that will make a significant impact on your organization.
Deploying lean principles requires a fundamental mindset of continuous improvement. One adjustment may not holistically reduce DNFB to a goal or baseline. However, successions of small improvements over time serve as a foundation to continue towards the goal.
As improvements are implemented over time, it can serve as a means to understand where automation can enhance lean processes and capabilities to reduce waste and enhance quality even further.
Want to make your revenue cycle department even more efficient? Find out how the AKASA platform and our unique approach to generative AI-powered automation can help your organization streamline RCM workflows. Schedule a free demo today.
AKASA
Oct 12, 2021
AKASA is the preeminent provider of generative AI solutions for the healthcare revenue cycle.









