Leveraging first pass payments as a key metric instead can more accurately forecast performance, according to revenue cycle automation experts at AKASA
AKASA™, the only Unified Automation™ company for healthcare revenue cycle management, today released survey results demonstrating that measuring the difference between clean claims and initial denials rates has become standard practice for revenue cycle operations teams at health systems across the country.
Revenue cycle automation experts at AKASA recommend health systems instead focus on first pass payments as the main key performance indicator. This measures the true outcome of claim preparation practices and accuracy.
“In my experience, metrics like clean claims can lead executives to believe they are performing better than they actually are, only to see their rate of initial denials is still high,” said Amy Raymond, Head of Revenue Cycle Operations at AKASA. “Shifting the organization’s focus to actively manage performance against first pass payments provides one metric that accurately measures performance. Efforts to improve first pass payments will by default also improve clean claims and initial denial metrics as well.”
Clean claims refer to claims that are considered error-free and expected to be ready for processing and payment by payors or insurance companies and organizations. Initial denial rates refer to the percentage of claims submitted to payors that are initially denied for any number of reasons. In theory, if 90% of an organization’s claims are “clean”, then 90% of their claims should be paid on the first pass or the first time they are submitted to a payor.
“Employing automation isn’t just about increasing productivity,” said Malinka Walaliyadde, co-founder and CEO of AKASA. “Leveraging effective automation solutions should also improve accuracy, which translates into optimal results. For hospitals and health systems, this means financial automation strategies should directly expand revenue capture, elevate the nature of work for their staff, and enhance operations.”
Commissioned by AKASA, the survey fielded responses from more than 350 chief financial officers and revenue cycle leaders at hospitals and health systems across the United States through the Healthcare Financial Management Association’s (HFMA) Pulse Survey program between December 17, 2020 and February 5, 2021. The national survey was designed to assess the adoption of automation in revenue cycle operations at hospitals and health systems across the U.S.
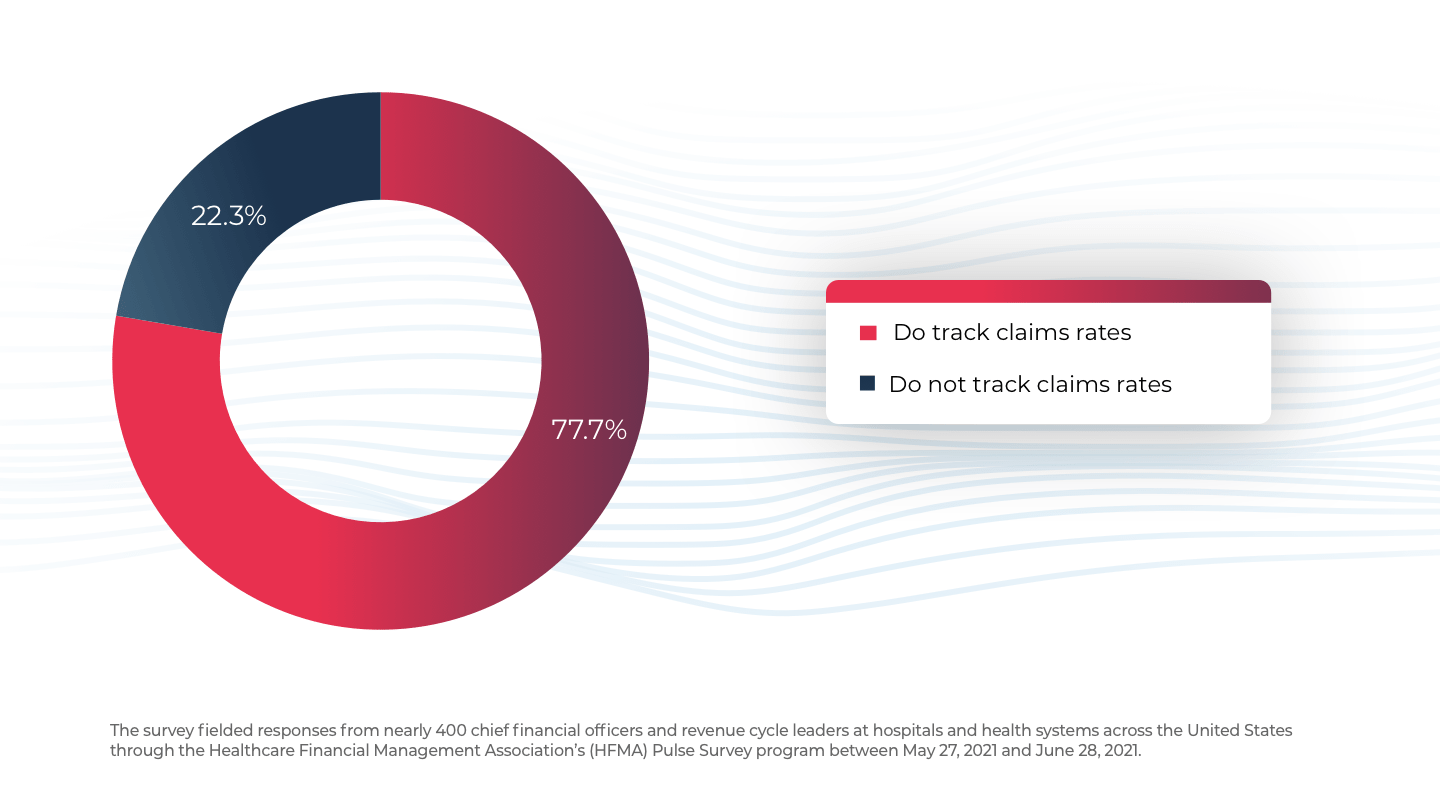
Survey respondents were asked
Does your organization track the difference between your clean claims rate and your rate of initial denials?
About AKASA
At AKASA, we believe every dollar spent on healthcare matters because healthcare matters to everyone. The only Unified Automation™ company for healthcare, AKASA uses the same machine learning approaches that made driverless cars possible to provide health systems with a single solution for automating revenue cycle operations. AKASA’s unique expert-in-the-loop approach, Unified Automation, combines modern machine-learning with human judgment and subject matter expertise to provide robust and resilient automation. Unified Automation™ adapts to the highly dynamic nature of revenue cycle operations and has been purpose-built for healthcare. AKASA enables health systems to decrease their cost to collect so they can invest more in patient care and be better stewards of the healthcare dollar. AKASA is based in the heart of Silicon Valley. Learn more at www.AKASA.com.

