Your RCM Success Kit includes:

Report | Solving Today's Greatest RCM Staffing Challenges
Brochure | AKASA + Cerner

Video | AKASA automation demo
Webinar | How University Health started their automation journey
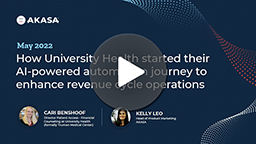
Case Study | How Methodist Health System automated at-risk and past-due claims
How we've helped other Cerner customers
78% of health systems are using or implementing revenue cycle automation
Automation is now mission-critical for driving efficiency and cost-effectiveness in healthcare operations.
71.3%
of accounts removed from queues
86%
efficiency improvement in claims
50%
of eligibility denials rebilled to payers
The AKASA revenue cycle automation solution
Auth Determination & Initiation
Resolve more prior authorizations and enable timely patient care by ensuring auth requests are thorough and accurate.
Auth Status Check
Improve prior authorization turnaround time by getting well-timed auth statuses to drive follow-up workflows.

Comprehensive Claim Status
Speed up claim resolution by automatically obtaining up-to-date status info for submitted claims.
Claim Attachment Resolution
Expedite claims processing by accurately identifying, retrieving, and submitting solicited documentation to payers.
We're excited to team up with AKASA to accelerate the adoption of advanced automation within the revenue cycle. Through our work together, our goal is to enable providers to more easily access and benefit from advanced Al-powered revenue cycle workflow automation.
Steve Colucci — Vice President, Revenue Cycle at Oracle Cerner