The Gist
Claim volumes are on the upswing, while hospitals continue to face high staff turnover and new payer rules and regulations — bringing the need for automation to the forefront. Read on to learn how an academic medical center faced an increase in volume due to Medicaid expansion and turned to automation to help — and what they learned along the way
Healthcare revenue cycle management in the United States continues to be plagued by a host of challenges that affect an organization’s operations, efficiency, and profitability.
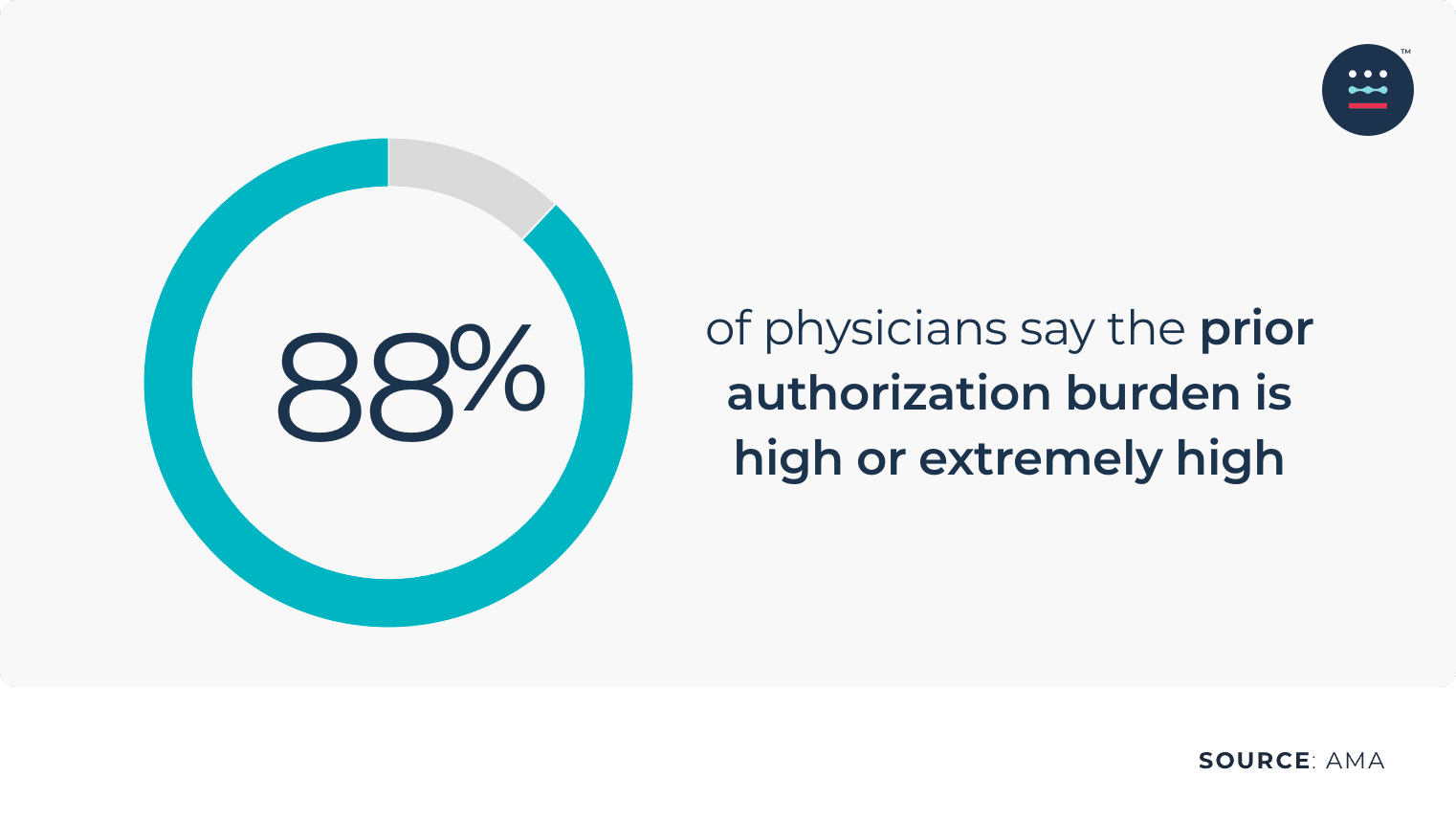
For starters, payer complexity is increasing. In fact, 83% of physicians say that the number of prior authorizations needed for prescription medications and medical services has increased over the last five years, according to a report by the AMA. And 88% of physicians describe the burden associated with prior authorizations as high or extremely high
As more patients return for procedures that were delayed due to COVID-19 concerns, outpatient volumes are also steadily increasing.
The latest data from Kaufman Hall’s National Hospital Flash Report showed a 16.1% month-over-month increase in outpatient revenue compared to February 2020 and a 34.9% increase compared to March 2020.
At the same time, The Great Resignation shows no signs of slowing down, with staff turnover rates at 30%, according to the American Hospital Association (AHA).
To address some of these challenges, Becker’s Hospital Review recently hosted an AKASA-sponsored webinar: “How University Health Started Their AI-powered Automation Journey To Enhance Revenue Cycle Operations.”
The webinar was co-presented by:
- Kelly Leo, Head of Product Marketing at AKASA
- Cari Benshoof, Director Patient Access – Financial Counseling at University Health.
Benshoof shares how she got started with AI-based automation, how she scoped her efforts, and recommendations for other organizations thinking of doing the same.
Here, we summarize eight key takeaways that revenue cycle leaders can use to get started with automation, increase efficiency, and drive revenue.
1. Not All Automation Is the Same
Automation is often used as a bucket term, but there are several types of automation used within healthcare operations and the revenue cycle, with various benefits and use cases. These include:
Robotic Process Automation (RPA)
RPA is best for simple, linear, repetitive, and rules-based tasks. Despite its limitations, RPA is often used in areas that are too complex or dynamic for its capabilities. Also, RPA breaks, requires maintenance, has hidden costs, and cannot scale.
RPA + Artificial Intelligence (AI)
This automation combination provides intelligence but lacks responsiveness and resiliency. It’s often used to extract data from insurance cards or train algorithms on data processing.
RPA + Machine Learning (ML) + “Human-in-the-Loop”
This is the most robust combination of automation. ML is a subset of AI and can modify itself when exposed to more data. With the human-in-the-loop approach, the automation operates similar to a self-driving car in a busy city: it can navigate decision points and obstacles because a human steps in.
Revenue cycle experts train the model and intervene when the machine has encountered something it hasn’t seen before. It not only solves the task, but it goes back and trains the machine for future occurrences.
“This enables the machine to take on increasingly complex tasks over time while being flexible enough to make sure the claims are still being processed without interruption,” Leo said.
This type of automation also handles unexpected occurrences, is resilient and can take on complex workflows, and allows staff to focus on meaningful, high-value tasks.
2. Set Goals
Before starting with automation, it’s important to have a goal. For University Health, an academic medical center based in Kansas City, Missouri that provides quality care for those with the best insurance and those with no insurance at all, an opportunity for patients who newly qualified for Medicaid presented unique challenges.
Unlike other hospitals in the state, their payer mix was 27% Medicaid and 22% self-pay.
They also knew that in the midst of Medicaid Expansion in Missouri, they would have a high number of patients who were going to transition from their financial assistance program or self-pay to Medicaid Managed Care Plans.
As a result, they needed to prepare for the increased volume and handle the additional steps. But they also were faced with challenges such as manual intervention and needing more staff to help with the process, so they knew automation was necessary.
Our goal was to be able to manage what we knew we were going to have — an increase in volume — without adding staff to that process.
~ Cari Benshoof, Director Patient Access – Financial Counseling at University Health.
3. Start Small
With a new automation solution, it’s important to start with small projects and scale later. This helps you get the right processes in place and show early wins.
University Health started with prior authorization with one work list and three portals and then expanded to inpatient notifications for one payer.
Today, they’re working to expand the automation for additional payers and work lists, and adding automation for eligibility.
Work with your automation partner to select the best place to start. The right partner can help you evaluate your processes and queues and figure out if you should start with something small, the biggest pain point, the largest backlog, etc.
“AKASA spent a lot of time getting to know us, analyzing our data, analyzing our claims, analyzing our remits, so that they understood who we are and how they could best help us with our process,” said Benshoof.
4. Work With a Flexible Partner
Before deploying automation, it’s important to find a partner that will take the time to understand a hospital’s revenue cycle operations, and be able to handle complex workflows and changes, such as in the payer portals and the EHR.
It’s also important for the RCM automation provider to understand an organization’s unique needs, processes, and workflows, and be willing to work through a tailored process and provide SMEs as a resource.
Read more about choosing the right RCM automation vendor.
“The human-in-the-loop is really important to help us know quickly that a change has been made and not cause us unnecessary delays or denials of authorizations because of a change that’s been made within either a payer portal or within our EHR,” Benshoof said.
Frequent communications and feedback are also important to address issues that may come up.
5. Ensure Compatibility With Your Technology
Does your automation solution work well with your EHR or PMS? Everything needs to connect in order to be a truly effective option.
University Health runs its revenue cycle on Cerner. When Benshoof turned to AKASA as an RCM partner, she quickly got the Cerner team involved in the sales and implementation process. Bringing in all of her partners together helped everything run more smoothly and effectively. As an added bonus, AKASA and Cerner are already collaborating to power AI-based automation within the revenue cycle for providers.
6. Prepare Staff and Get Buy-In for Automation
Change management can be challenging, so before starting with automation, it’s important for organizations to be upfront and honest about the goals, the “why” of automation, the benefits, and the value.
“For us, we had a pretty clear story. We wanted to be able to explain to [our employees] that we did not want to necessarily decrease staff, but our goal was to not have to hire additional staff as Medicaid expanded,” Benshoof said.
After automation is up and running, it’s crucial that staff provide feedback about what’s working and what’s not.
7. Automation Isn’t Instant
While automation is effective, efficient, and saves time, it’s important for revenue cycle leaders to recognize that getting up to speed also takes time — and requires trial and error, communication, and feedback.
“Understanding that it’s machine learning and it’s going to take time to work through those bugs and those kinks is really important,” Benshoof said.
8. Know Your KPIs
Revenue cycle leaders will be focused on the key metrics, and with automation, it’s important to measure the right activity at the right time, Leo said.
Organizations should start off with the baseline data and then quantify the activity with metrics like volume automated and hours automated.
Then, they can measure the impact on their team, which can include metrics like reduction in time per task and percent decrease in denials.
Later, outcomes can be measured such as reducing cost to collect, days in A/R, and increase in revenue.
Want to learn more about how your organization can benefit from automation? Request a demo.