The Gist
Automating the healthcare revenue cycle was once thought impossible. Now, automation is increasingly popular and feasible. How did we get here, and what's next for healthcare?
Over the last 18 to 24 months, health systems have been rapidly introduced to the concept of process automation in several key functional areas including the revenue cycle. The shift in market awareness and appetite for automation has been dramatic. In 2018, as I was sharing revenue cycle best practices with leading health systems across the country, I can count on two hands the number of times that the topic of automation came up. Compare that to the second half of 2019, where over 50% of all progressive health systems that I have spoken with are currently pursuing automation or are actively evaluating it. The unforeseen paradigm shift that we are experiencing now in 2020 will only intensify the need. Health system leaders will need to come up with an automation strategy to deliver more effective performance at lower costs, but that strategy must start with a plan to navigate the array of automation options that are cropping up.
In 2018, as I was sharing revenue cycle best practices with leading health systems across the country, I can count on two hands the number of times that the topic of automation came up. Compare that to the second half of 2019, where over 50% of all progressive health systems that I have spoken with are currently pursuing automation or are actively evaluating it. The unforeseen paradigm shift that we are experiencing now in 2020 will only intensify the need. ~ Ben Beadle-Ryby - Sr. VP of Sales and Customer Success and Co-founder at AKASA
Most automation providers use robotic process automation (RPA), a tried-and-true but simple form of automation. While great at handling linear tasks, RPA on its own struggles to work within healthcare for two reasons:
RPA doesn't learn or adapt: RPA is like an Excel macro in that it works best in structured, stationary environments. While there is value in applying RPA to basic processes, its limitations cause it to break altogether when tackling dynamic areas like the revenue cycle. This leaves your team scrambling to complete work while bots are fixed by the vendor.
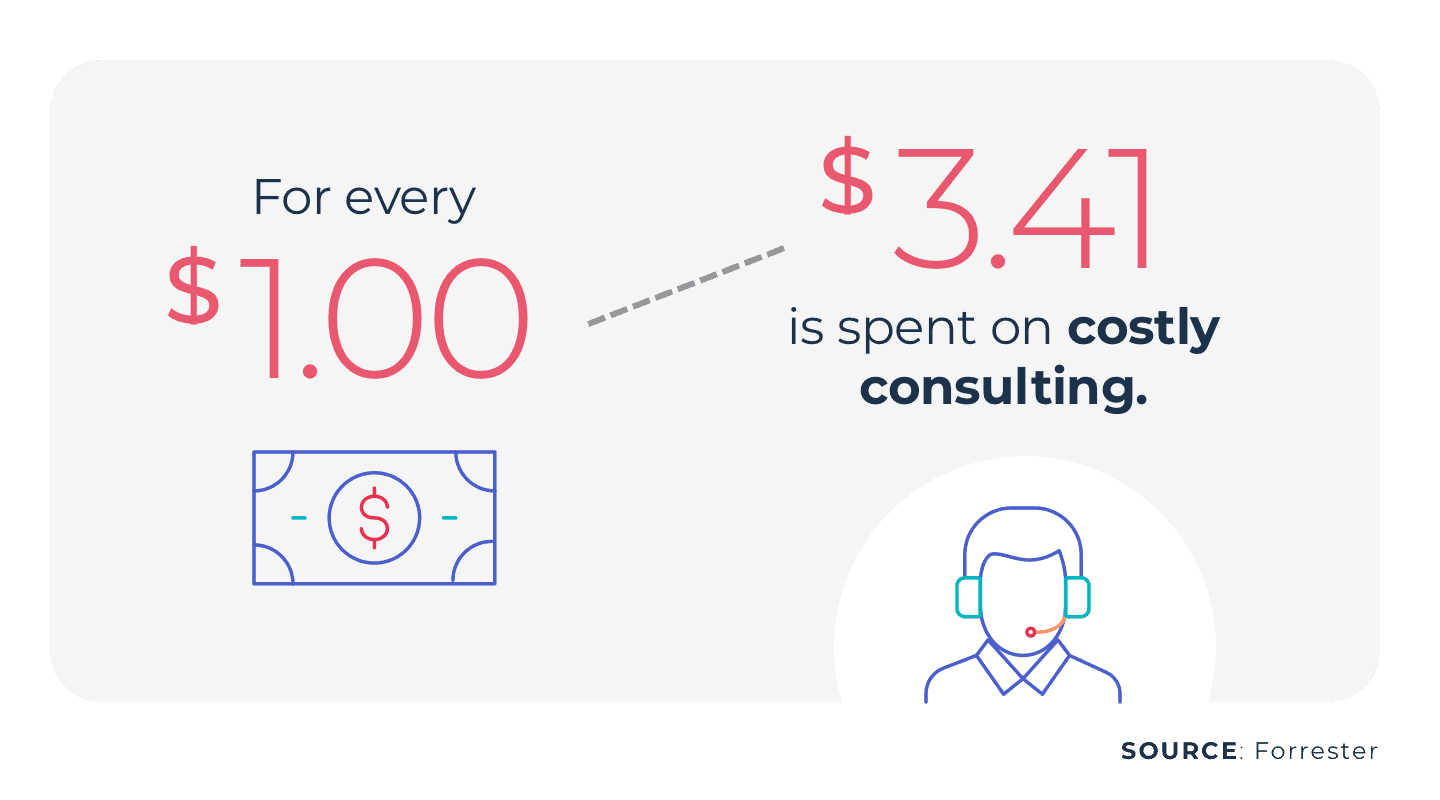
RPA has hidden costs: Because RPA does not learn or adapt on its own, it not only has to be manually built and programmed by teams or consultants, it also has to be maintained and repeatedly rebuilt by those staffing resources. What this means is that there are many hidden costs that go well beyond the cost of the original bot.
Again, RPA on its own is a cost-effective way to automate simple tasks. But, the healthcare revenue cycle is anything but simple, with edge cases frequently appearing and workflows often changing. In short: RPA needs help.
The Best Practice Approach: Unified Automation®
The best practice approach to automating workflows and existing staff processes is to partner with a firm that:
Has deep healthcare and revenue cycle domain experience
Leverages modern machine learning
Ensures consistent, high-quality results even amidst changing environments.
At AKASA, we've pioneered Unified Automation for healthcare revenue cycle management. Unified Automation runs on a foundation of RPA, but takes it a step further using leading-edge AI, machine learning (ML), and human experts-in-the-loop. By leveraging AI and ML, our automation continuously learns as it performs work. And, if it encounters an edge case, our dedicated team of revenue cycle experts complete the work and train the AI to handle that task. Unified Automation aims to streamline much of the revenue cycle and give revenue specialists the breathing room they need to thrive. But, there are also steps you can take on your end to help your revenue cycle run more smoothly.
Start With Your Highest Return Opportunities
Many of our clients ask us where they should start. There's a myriad of tasks and functions that are performed across the revenue cycle, so it's understandably difficult to prioritize the right ones. As a result, we completed an in-depth data-driven analysis to support health systems in pursuing the highest yield opportunities for automation for revenue cycle. Taking into account the complexity of each revenue cycle task, the current resources dedicated to it, and the role it plays in supporting the reimbursement process. We were able to boil down the results of that analysis to this: Finance and revenue cycle leaders should prioritize the following four areas for automation in order to achieve the greatest efficiency: 1. Eligibility Driven Off Of Patient Insurance Cards: Leverage machine learning to automatically input insurance card scans into your registration/EMR system fields and check eligibility on the front and back end of revenue cycle. This will prevent denials and reduce rework out of the business office. 2. Prior Authorization: Identify authorization requirements, initiate authorization via payer websites, and check authorization status to ensure your patient is fully supported by their third-party coverage to receive their care with full reimbursement. Today, authorizations are one of the leading causes of denials, so this will prevent denials and reduce back-end work associated with denials appeals. 3. Follow Up to No Payer Response and Claim Status: Complete follow up to claims with no payer response by checking the claim status on payer websites, pulling back relevant information into EHR/PAS, and prioritizing the need for escalation with the payer. This will drive down your A/R and increase your cash flow. 4. Denials Management -- Appeals, Adjustments, and Rebills: Automatically appeal technical or clinical denials by pulling the relevant clinical data from the EHR and applying the most effective appeals templates. Where adjustment is required due to managed care requirements or accounting practices, automatically perform that task and free up your team to tackle the meaningful, revenue-generating activities. This should decrease your overall write-offs rate and increase your collections. These four areas will be the biggest drivers in lowering your cost to collect and will ultimately be the foundation for achieving a cost to collect well below current industry standards of 3% and achieve new industry best practices, as we discussed in our post, "The Revenue Cycle of the Future."
Following Top Priorities, Expand to Other Revenue Cycle Tasks
After health systems have automated these areas and achieved improved performance with lower overall costs, there remains many opportunities to expand automation to other functions in the revenue cycle. Here are some additional critical tasks ideal for automation:
Claim/Bill edits
Cash posting
Price estimation and patient out-of-pocket responsibility
Payment variances including underpayments
Medical necessity check
Charge reconciliation
Coding
Clinical documentation improvement
For all of these items, it should not just be a basic bot that runs through the same click path every time. Every action should be driven off of an advanced algorithm that can statistically show how the action will reduce the likelihood of denials.
The Goal of Automation
At the end of the day, automation should not only reduce your costs, it should also improve the accuracy of the work completed and improve performance against your key performance indicators. Automation can:
Ensure that you are multiple days out on verifications, authorizations, and medical necessity and, ultimately, prevent denials for technical reasons.
Accelerate the time to payment.
Enable your patient financial experience efforts by engaging your patient's insurance card and fast-tracking the eligibility and out-of-pocket estimate process.
At AKASA, Unified Automation delivers the most comprehensive performance for the healthcare revenue cycle. At the end of the day, this type of automation is not just about cost reduction, it's about improving your revenue cycle performance holistically. It is the key component to achieving the revenue cycle of the future. To see how Unified Automation can help your organization step into the future, schedule a free demo today.
AKASA
Jun 4, 2020
AKASA is the preeminent provider of generative AI solutions for the healthcare revenue cycle.









