The Gist
Revenue cycle management automation is necessary to handle the complexity of tasks, ranging from patient eligibility determinations to denials management. There are several key steps providers can take to make their RCM automation more durable and efficient.
Revenue cycle management (RCM) automation has become a top priority for providers. With the decline in patient volumes and revenue due to the COVID 19 pandemic, plus the shift to remote work, only a highly automated revenue cycle can ensure a consistently short path to payment. Truly intelligent automation can scale to the vast number of tasks across the revenue cycle, while also adapting to inevitable changes in systems, interfaces, and regulations.
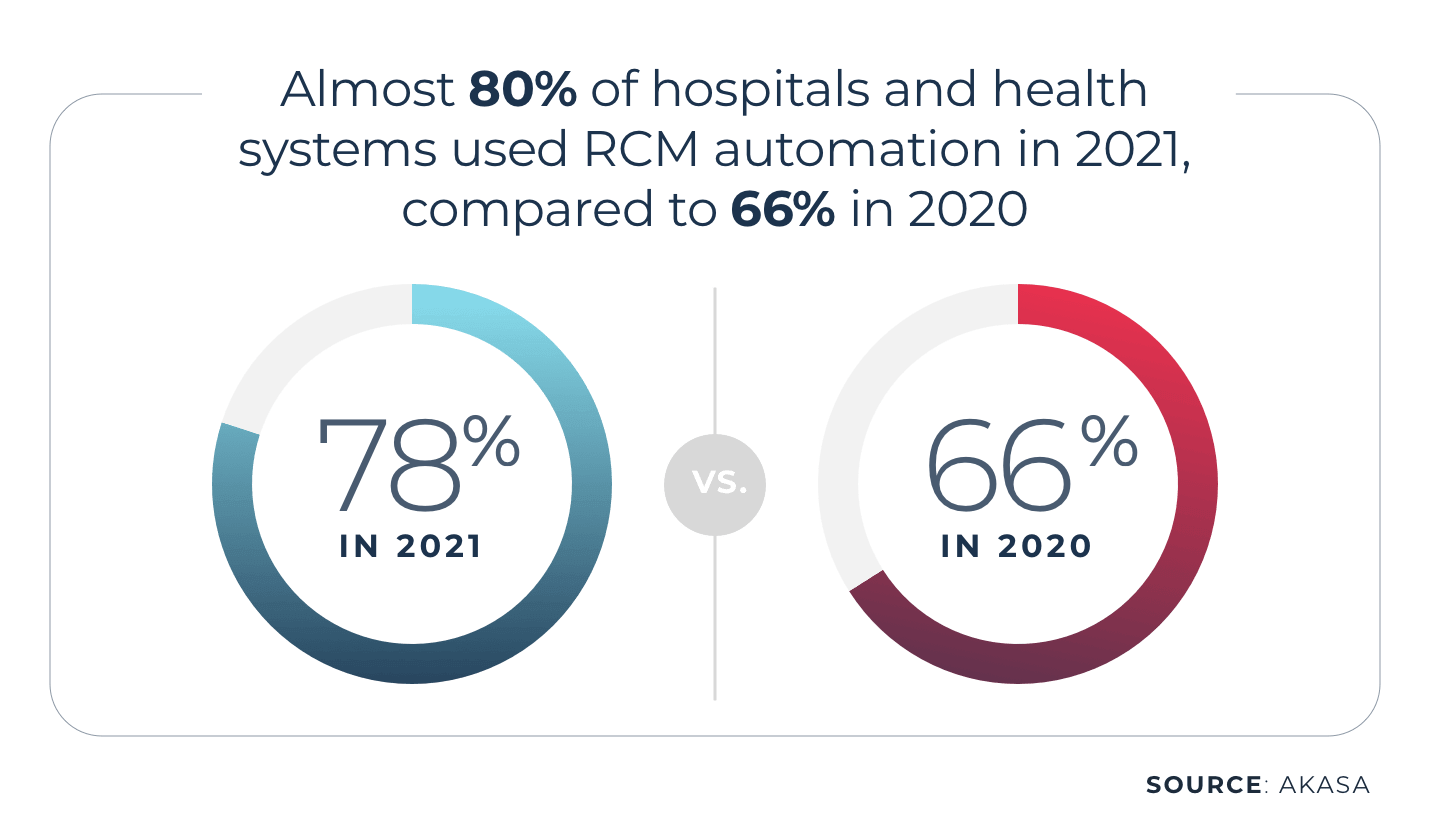
For these reasons, almost 80% of hospitals and health systems used some form of RCM automation in 2021, compared to 66% in 2020, according to an AKASA survey.
Revenue cycle automation isn’t new, and it comes in multiple forms. Some of them — like the limited automation provided in electronic health records (EHR) and robotic process automation (RPA) — are relatively old. Choosing the correct type of automation, as well as formulating a strategy for supporting and sustaining it, is essential to maximizing revenue cycle efficiency.
Effective automation is vital for healthcare leaders looking to truly optimize their RCM processes, increase efficiencies, and lower cost to collect. But it’s important to be thorough and find the right automation platform and partner that can help your unique operations succeed.
~ Amy Raymond, VP of Revenue Cycle Operations at AKASA
Let’s look at four steps toward better revenue cycle management automation.
Step 1: Go Beyond Bolt-on and Fragile Automation Solutions
The history of revenue cycle automation stretches back decades to the rollout of staff augmentation initiatives that used spreadsheets to integrate and organize data — a critical step beyond the fully manual healthcare revenue cycle management processes that preceded it.
From there, healthcare organizations began to partially automate revenue cycle operations via solutions that bolted onto their then-new EHRs or enterprise resource planning (ERP) systems through RPA.
Neither approach is ideal:
- EHR and ERP additions can be costly to purchase and implement. Moreover, they might not be specifically designed for the revenue cycle, limiting their effectiveness. Decision-makers have to pick carefully among many different options and then maintain them over time.
- Stand-alone RPA is an old technology from the early 2000s. Although it can automate some simple, straightforward tasks, extensive manual preparation and troubleshooting are often required to script the different bots and take action if they break. The frequent changes in payer systems, rules, and regulations make RPA challenging to scale.
Hospitals and healthcare systems need something more robust.
This is where artificial intelligence (AI) and machine learning (ML) enter the picture, as resilient forms of revenue cycle automation that actively adapt to changing conditions.
Step 2: Use Artificial Intelligence and Machine Learning for Purpose-Built Automation
Unlike traditional RPA or either EHR or ERP additions, AKASA’s solutions for revenue cycle management automation incorporate leading-edge AI and ML and are built specifically for healthcare use cases. The best solutions integrate with and operate within the same medical billing and EHR systems that revenue staff already use.
AKASA has created a unique platform called Unified Automation® that is purpose–built for healthcare. It scales human intelligence with leading-edge AI and ML trained on customer data to learn unique systems, continuously adapt to changing environments, and deliver comprehensive automation and analytics for complex workflows.
After initial setup, the platform will observe existing tasks, like eligibility verification, and then learn and perform them. This process allows for the creation of complex workflows that would never be scriptable by hand.
For example, dealing with denials management through RPA can require writing literally hundreds of healthcare RCM rules to handle a wide range of scenarios. With AI and ML, such manual effort is not required, as the solution will automatically see what is happening in each scenario (or workflow).
The adaptability of the AI and ML approach to revenue cycle management automation is vital in light of modern revenue operations’ complicated and dynamic state.
Ongoing trends such as the rise in patient payment responsibility, the growing scrutiny of surprise billing practices, and the increase in remote work all put pressure on providers to keep pace with substantial change. Doing so is easier if repetitive and time-consuming revenue cycle tasks don’t have to be managed by hand or with fragile tools requiring lots of attention.
Step 3: Simplify Automation Solution Upkeep
What happens after a hospital or health system has implemented revenue cycle management automation?
The answer varies depending on the type of automation chosen.
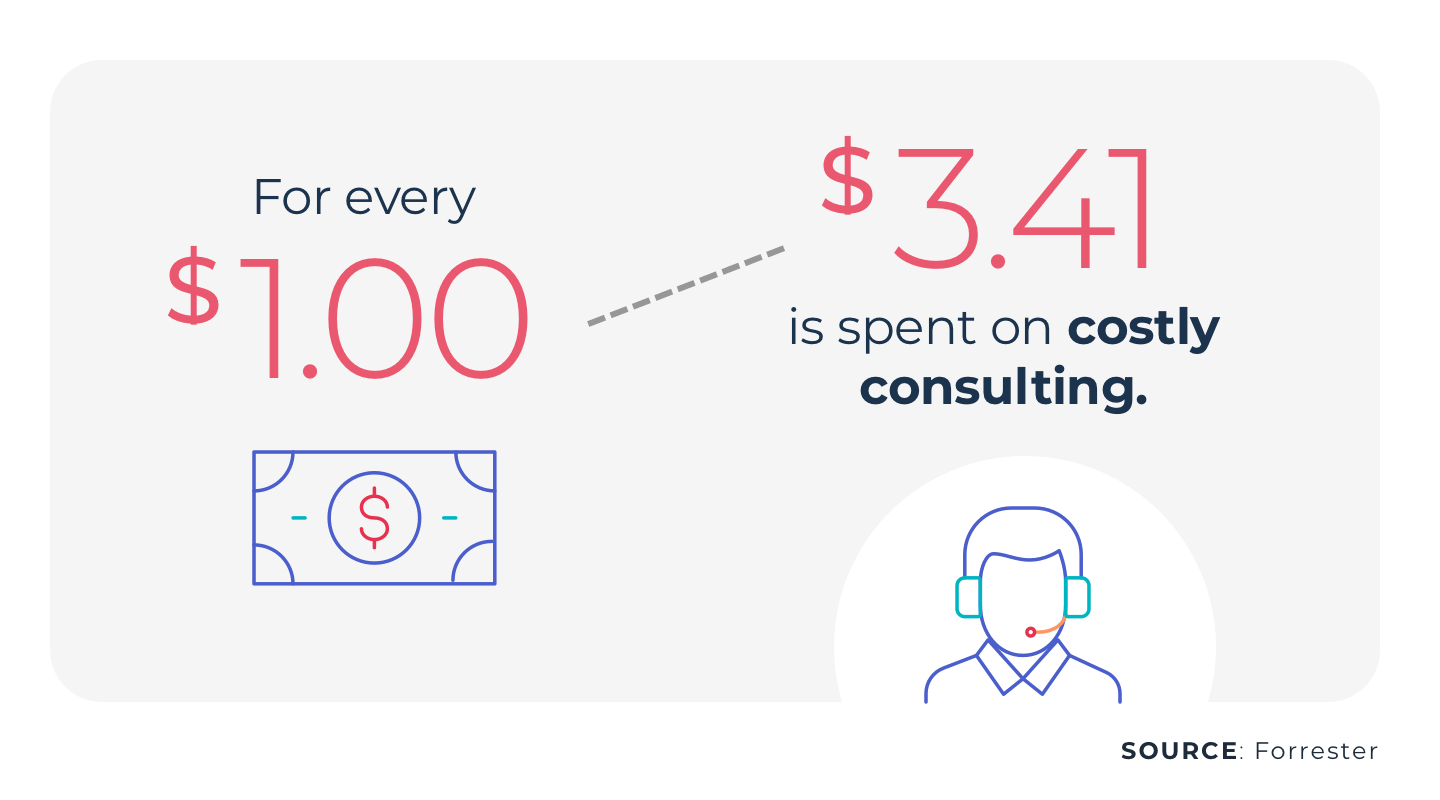
If the healthcare organization has opted for EHR or ERP bolt-ons, or for traditional RPA, then the future could involve numerous meetings with consultants and a creeping budget to fix broken systems and bots. Not to mention the staff time often needed to work exception cases and RPA errors (or exception cases and babysit the RPA). The costs and lost time involved may negate many of the advantages of trying to automate tasks like prior authorization, eligibility checks, and denials management.
In contrast, AKASA’s AI and ML path has been carved with outliers in mind. The complexity of the revenue cycle means that there will always be at least a handful of situations that even well-trained AI and ML won’t be able to handle in one pass — which is why a human-in-the-loop approach is essential.
When the AKASA system identifies an outlier, an AKASA RCO expert can immediately take on these edge cases, resolve them, and ensure that the AI and ML engines learn from the incident. Accordingly, long-term upkeep is easier.
“This blend of human judgment and automated technology is the only way to address the overall complexity of the revenue cycle process,” explains Raymond. “AI and machine learning handle the lion’s share of claims, while human experts are always available to work the more unusual ones and then imprint their expertise into the automation itself.”
Step 4: Don’t Overdo it on Technology
“Less is more” is a cliche, and one that might not seem evident in the healthcare technology world, in which there are a plethora of tools targeted at a wide range of use cases, including revenue cycle workflow automation.
But the Healthcare Financial Management Association (HFMA) has offered useful guidance on how to select and prune revenue cycle tools, with an eye toward quality instead of quantity.
HFMA has highlighted the need to get “higher-than-linear yields” from RCM automation solutions, meaning that any tool should be transformative and not iterative. Plugging gaps with traditional RPA or bolt-ons will at best only give linear improvement, once factoring in the time required for deployment and upkeep of each solution.
Seek exponential yields through intelligent automation that evolves alongside the revenue cycle itself and can also:
- Be deployed quickly and remotely, without numerous consultants
- Integrate tightly with all the important billing and EHR systems in use
- Be developed and improved by credentialed AI and ML experts
- Include true revenue cycle leadership and expertise
These attributes shorten the time to value for revenue cycle leaders as part of Unified Automation. AKASA uses this platform to combine healthcare-specific AI and machine learning with subject matter experts to deliver a unique revenue cycle solution. The result is a seamlessly integrated, customized solution that reduces operating costs and helps health systems allocate resources where they matter most.
Learn more about how AKASA can make your revenue cycle more efficient by scheduling a demo.