The Gist
RCM healthcare automation often promises to solve many of the challenges in the revenue cycle (claims payment, etc.). Unfortunately, the common solution of RPA doesn’t always provide the truly resilient automation that organizations need. For that, you need AI and ML-based technology that enables advanced, adaptive automation and is well-suited to dynamic environments.
In healthcare, revenue cycle management (RCM) encompasses all of the steps a provider — a hospital or health system — takes to track and collect revenue related to patient encounters.
An RCM healthcare workflow begins as early as when the patient schedules an appointment. It then proceeds through actions, such as payer communications, usage of medical billing systems, and collections from insurers and patients.
Given the overall complexity of the revenue cycle and the time required for managing it manually, RCM healthcare automation has been a long-term goal for healthcare organizations.
Effective automation is proving key in truly optimizing RCM processes, increasing efficiencies, and lowering the cost to collect through consistent and optimal execution of workflows.
~ Amy Raymond, head of revenue cycle operations at AKASA
But past automation technologies haven’t always lived up to their promise, falling short of solving some of the overarching challenges in realizing revenue.
Major Challenges in Healthcare Revenue Cycle Management
The top metrics for revenue cycle management are evolving, according to a new study from AKASA. Benchmarks such as the number of days a claim lingers in accounts receivable, the number of outstanding unpaid patients bills 90+ days past due, and initial denial rate have emerged as the key performance indicators that financial leaders care about. Healthcare systems need to evolve their strategies to focus on those metrics.
A November 2019 Medical Group Management Association survey found that almost half (48%) of revenue leaders identified “claims payment” as their top revenue challenge. Other widely cited issues across the revenue cycle included prior authorization, denials management, and staffing. These are all major obstacles that RCM healthcare automation should, in theory, be able to address.
But, in reality, the typical provider relies on a patchwork of solutions that don’t deliver truly resilient automation. From medical billing to receiving reimbursement, healthcare organizations often use fragile, linear robotic process automation (RPA) to manage previously manual revenue activities.
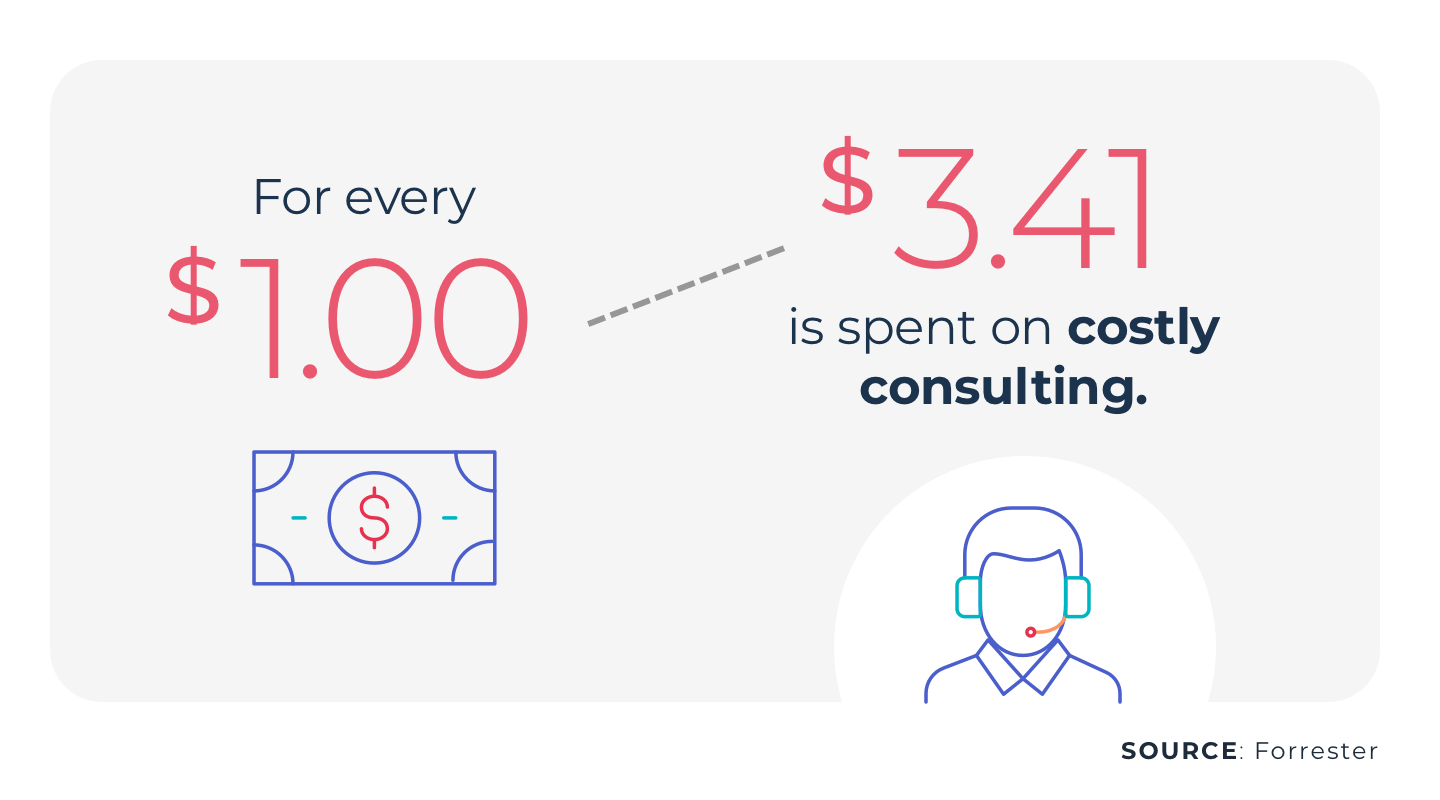
RPA works for some discrete and linear tasks, but breaks down when interfaces, codes, and pages change. Moreover, it doesn’t evolve. Meaning it can’t make intelligent determinations — like predicting how likely a claim is to be denied or learning which claims require follow-up. This often translates to expensive consultants and upkeep for traditional RPA.
For example, a revenue cycle leader from the University of Pittsburgh told Healthcare Innovation in 2021 that, throughout the 2010s, RPA had become the primary way his organization completed administrative tasks from payers within portals. However, his team was eyeing an upgrade to artificial intelligence (AI) and machine learning (ML) in the coming years.
As providers navigate challenges like the rise in telehealth services and growing patient responsibility for medical billing, automation is becoming more integral to the revenue cycle, while outsourcing also gains popularity.
AI and ML: A Better Approach to RCM Healthcare Automation
The logic behind this key RCM healthcare upgrade is simple: AI and ML enable advanced, adaptive automation that is well-suited to dynamic environments.
- AI refers to machines that can perform human-like tasks, such as visual perception
- ML is a subtype of AI that can improve its capabilities without human intervention
Predicting denials based on payer rules is a prime example of how AI and ML can achieve what RPA can’t. Automation built on these technologies continuously learns from data inputs — to the point that it can autonomously perform advanced revenue cycle management workflows, right from within the medical billing systems staff already use.
In other words, it adapts to new information and system updates, without requiring the frequent maintenance and overhead of RPA. When edge cases occur, the automation platform knows to hand them off to humans. Over time, AI and ML also become better at handling even these unusual tasks.
This is how AKASA’s Unified Automation® works.
It brings together AI, ML, and experts-in-the-loop, creating a single solution that proactively and autonomously navigates medical reimbursement. The result? More intelligent RCM healthcare automation, in support of better stewardship of the healthcare dollar.
Schedule a free demo to see Unified Automation in action and learn how it can help your organization.











