Your RCM Success Kit includes:

Report | Solving Today's Greatest RCM Staffing Challenges
Brochure | AKASA + Cerner

Video | AKASA automation demo
Webinar | How University Health started their automation journey
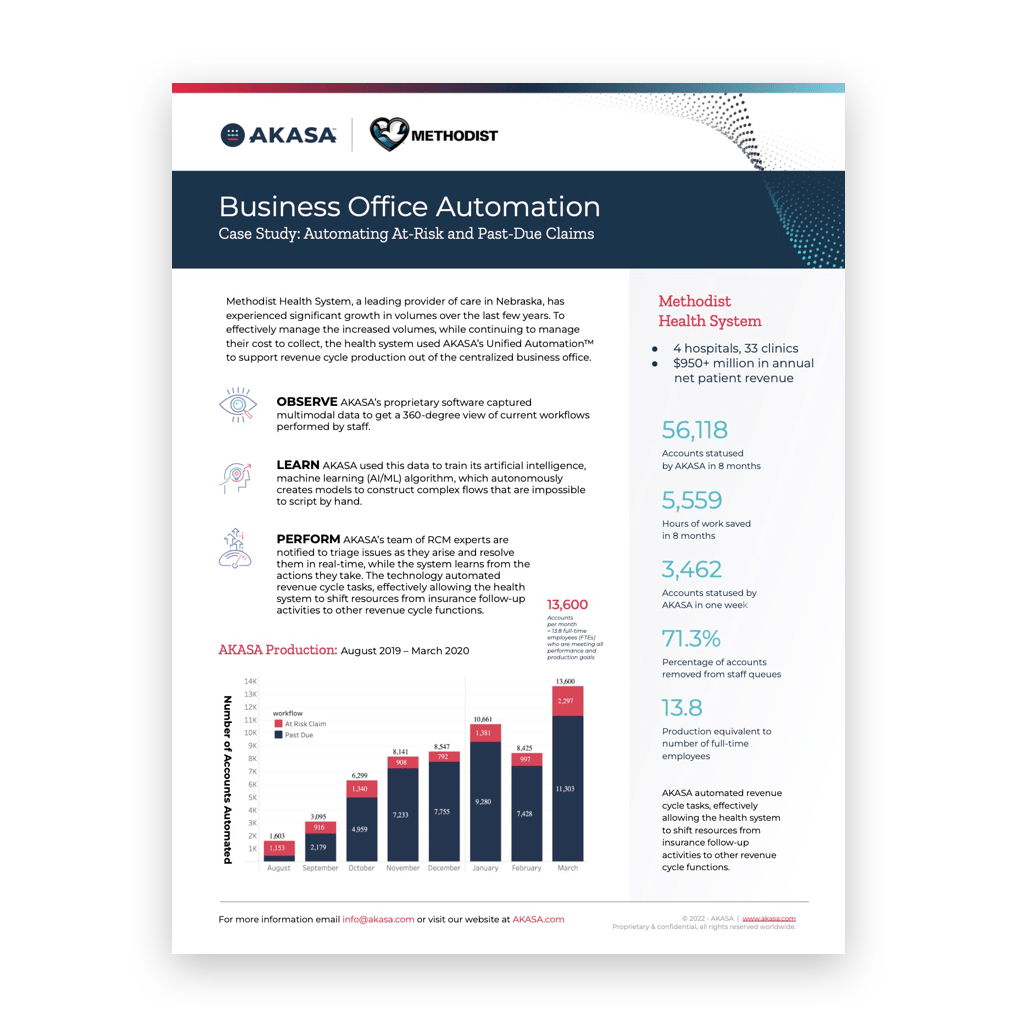
Case Study | How Methodist Health System automated at-risk and past-due claims
How we've helped other Cerner customers
78% of health systems are using or implementing revenue cycle automation
Automation is now mission-critical for driving efficiency and cost-effectiveness in healthcare operations.
71.3%
of accounts removed from queues
86%
efficiency improvement in claims
50%
of eligibility denials rebilled to payers
The AKASA revenue cycle automation solution
Auth Determination & Initiation
Resolve more prior authorizations and enable timely patient care by ensuring auth requests are thorough and accurate.
Auth Status Check
Improve prior authorization turnaround time by getting well-timed auth statuses to drive follow-up workflows.

Comprehensive Claim Status
Speed up claim resolution by automatically obtaining up-to-date status info for submitted claims.
Claim Attachment Resolution
Expedite claims processing by accurately identifying, retrieving, and submitting solicited documentation to payers.