The Gist
No two RCM automation providers are the same, but many make the same promise: the perfect fit. Knowing what to look for in an RCM automation provider is key to finding one that actually fits your operations.
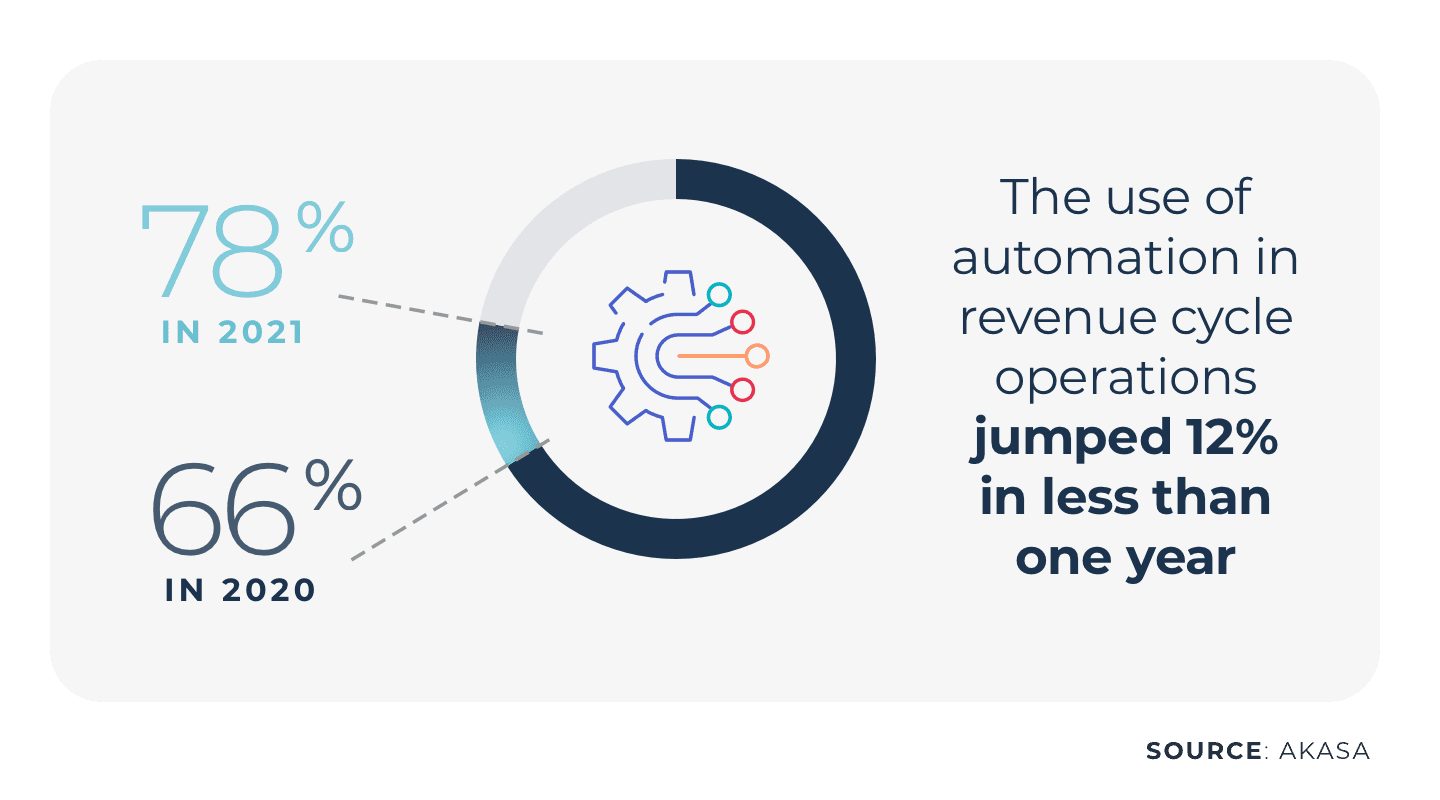
RCM automation efforts have been in use for some time now, though with varying abilities and to varying degrees. The use of automation in revenue cycle operations jumped 12% in less than one year, from 66% to 78%, according to an HFMA survey commissioned by AKASA
Of those organizations that don't use it, more than half said they plan to in the near future. Healthcare financial leaders need to streamline complex staff workflows. This not only improves the bottom line but can also increase patient and worker satisfaction. Patients experience a more streamlined billing cycle without as many surprises, errors, or needs to follow up on coverage. Workers are freed to work to the top of their skill set, reassigning mundane and time-consuming tasks to the automation partner and focusing on more complex tasks that demand human guidance. If you're looking at incorporating automation into your revenue cycle team, where should you start? What should you look for in an RCM automation provider?
Across my career, I've seen the increasing need for healthcare technology platforms that better engage the workforce, bill more accurately for reduced patient frustration, and eliminate tedious, redundant, and time-consuming work. Automation platforms that employ artificial intelligence (AI) and machine learning (ML), coupled with guiding expertise from industry veterans, are the best answer to helping us create the ideal revenue cycle of the future. ~ Grant Messick, VP of Customer Success at AKASA
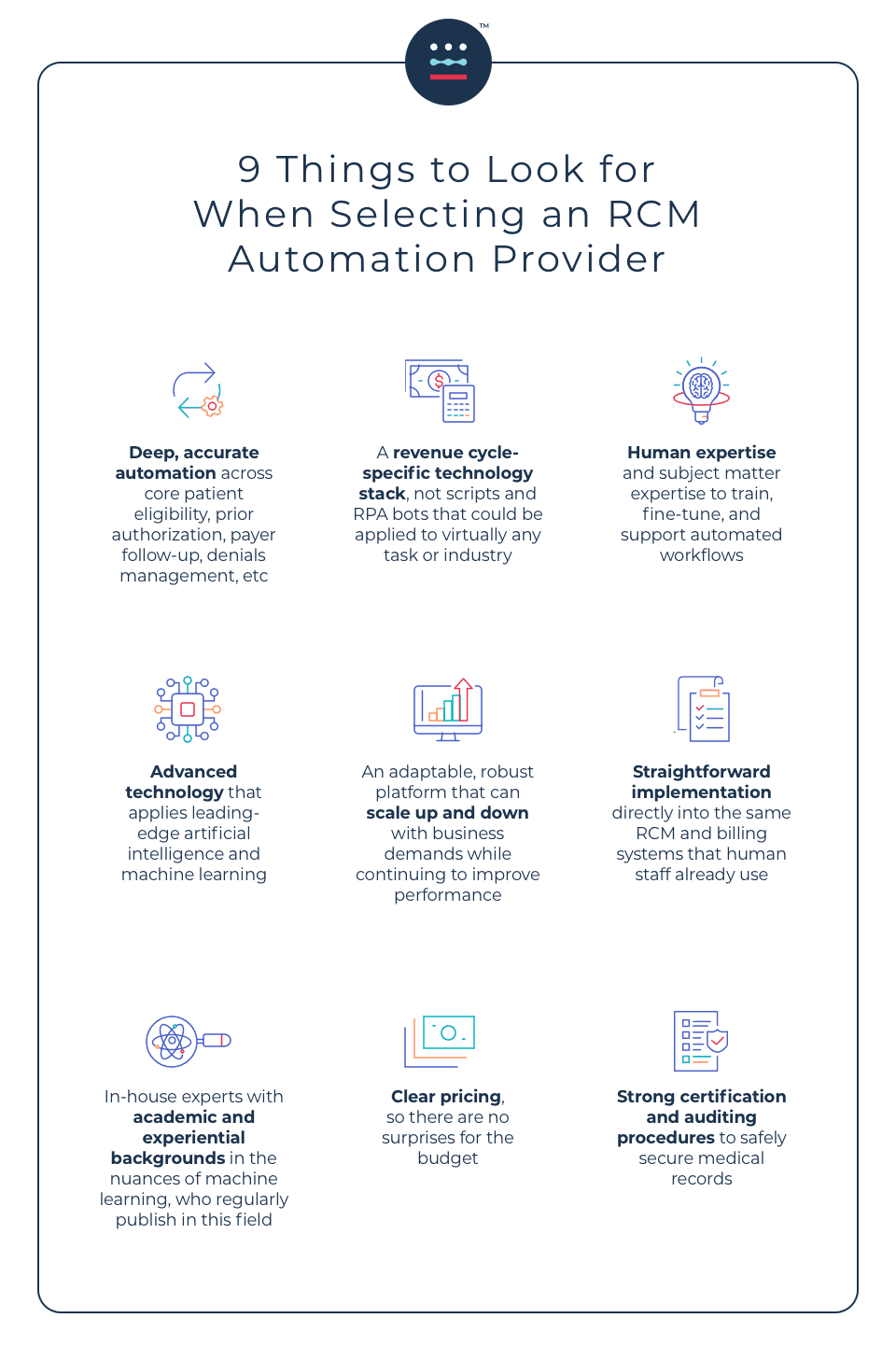
A future-focused RCM automation provider should have the following nine characteristics. If your partner and its platform are able to meet these criteria, your operations will run more efficiently, and you will drive more revenue for your organization.
1. Deep, Accurate Automation
It's important for revenue cycle automation providers to be able to handle more than one task and do so in such a way that improves the accuracy of the work completed. Look for solutions that work across the revenue cycle, rather than just one segment. Scalable platforms can help save money and time, and can require less overall human capital investment. Having capabilities across core patient eligibility, prior authorization, payer follow-up, and denials management functions are important, as these are areas that can quickly impact an organization's bottom line.
2. Revenue Cycle-Specific Technology Stack
Does the vendor understand your organization's specific needs and the needs of the revenue cycle industry? Robotic process automation (RPA) has largely been considered an established concept for automation efforts; however, these solutions employ scripts and bots that were developed for and can be used by a variety of industries. The developers often don't have knowledge specific to revenue cycle operations, and especially not the subset of healthcare revenue cycle operations. Some organizations also buy generic RPA toolkits and try to leverage their own talent and expertise to deploy them in healthcare. But it can be challenging and set your revenue cycle team even further back. Technology purpose-built for revenue cycle-focused tasks and EHRs understands the unique challenges of this industry, rather than being retrofitted for it.
3. Human Expertise
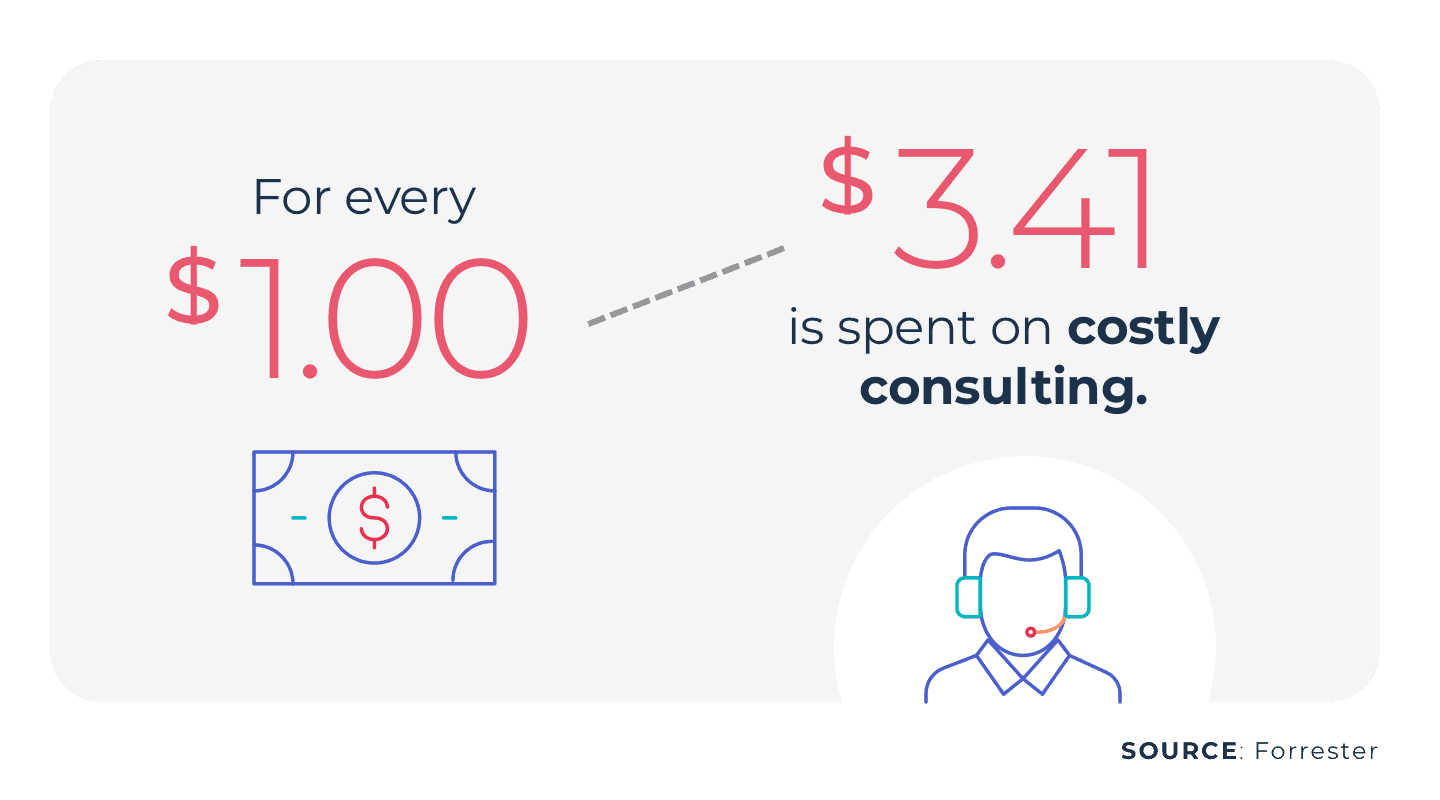
Human experience in the revenue cycle is imperative to build cost- and time-saving solutions. Bots are also inflexible and break easily, which can require expensive consulting to fix.
You can avoid this by looking for providers that integrate a human-in-the-loop approach. Platforms that continue to rely on humans for complex problem solving are more resilient. AKASA has built a unique platform called Unified Automation® that combines AI and ML with human revenue cycle experts. When the technology encounters an outlier or edge case, it triages it to an AKASA revenue cycle expert. The expert solves the problem and the technology learns from the expert. Then, if the issue comes up again, the technology can solve it independently. Keeping people working with the technology allows for expert handling of outliers that are inevitable in revenue cycle operations.
4. Advanced Technology
Is the RCM automation provider using the most up-to-date technology available? Yes, RPA can be useful in certain circumstances, such as solving linear problems. But the revenue cycle is rarely linear. It has complexities not found in many industries. Look for a technology partner who is using true AI and ML to solve complicated problems with advanced solutions. AKASA is the leading developer of AI for healthcare operations. The platform scales human intelligence with leading-edge AI and ML trained on customer data to learn unique systems, continuously adapt to changing environments, and deliver comprehensive automation and analytics for complex workflows.
I am proud to work with some of the best engineering minds in the country. They understand how to take the latest developments in machine learning and artificial intelligence and apply them to the real-world challenges of the healthcare revenue cycle. ~ Grant Messick, VP of Customer Success at AKASA
5. Scalable Solutions
One pain point that can be difficult to manage with any platform is business fluctuations. Seen or unseen, they most often cause many headaches: proactively planning and future-casting to ensure the right staffing mix and/or managing solutions that are not able to quickly flux with business flow. The right RCM automation provider should offer a platform that is adaptable and robust, while automatically scaling up and down with ease as business demands fluctuate -- expected or not. This helps avoid a staffing yo-yo situation, and allows revenue cycle operations to run smoothly year-round. AKASA's AI/ML + expert-in-the-loop approach expands the capabilities of automation to take on far more complex work and to do it at scale.
6. Straightforward Implementation
When choosing an RCM automation platform, you can either choose a new system that requires training to integrate into existing systems or a solution that offers direct implementation into the same RCM and billing systems that human staff already use. The latter requires a lower human capital investment and offers a faster integration timeline. The result is less confusion and more accurate workflows.
7. Academic and Experiential Background
At AKASA, we believe in bringing the same scientific rigor seen on the clinical side to healthcare operations. Automation is a complex field. It's important that any partner you work with has engineers and developers with a deep understanding of technology and healthcare revenue cycle management. Ask who will be maintaining your platform. What expertise do they bring? Are they experts in artificial intelligence and machine learning? Are they publishing in peer-reviewed journals? Your partner's system is only as strong as the expertise that builds and maintains it. You want seasoned professionals with experience constantly advising the team and ensuring your platform is optimized for your needs. For example, AKASA's engineering team regularly publishes and presents on high-level topics. Our research-first approach means that our customers have access to leading-edge technology. We are committed to publishing on our AI and approaches in peer-reviewed publications to continually set new state-of-the-art standards for AI in healthcare operations and to lead our entire industry forward. Read about AKASA's research on autonomous medical coding that was presented at the Machine Learning for Health Care Conference.
8. Clear Pricing Models
This should be the price of entry for any platform. Getting approval to onboard a revenue cycle automation partner is a strong first step to more accurate and smoother transactions. This should also apply to your partner of choice. Clear pricing models is a concept that should be embraced by both sides. If your potential partner is not able to provide this, it is a sign of potential trouble ahead. A partner who is confident in their platform and its appropriateness for your needs should have no trouble being open from the start. This helps you set up accurate and reliable financial expectations within your organization, as well as manage the budgets you set.
9. Strong Certification and Auditing Procedures
You take your responsibility to safely secure your patients' medical records -- your partner should too. Not only should a revenue cycle automation partner work within your existing ecosystems, abiding by your controls and creating audit trails in your systems, but it should also go above and beyond to ensure you remain compliant. There should be records of every action the platform takes and HIPAA and HITRUST compliant infrastructures, as well as the appropriate encryption for data in transit and data at rest. Read about AKASA's security and compliance efforts.
AKASA brings these nine components together with Unified Automation. We empower healthcare providers to automate their revenue cycle operations with a combination of AI, ML, and humans. Learn how AKASA can make your processes more efficient by requesting a demo.
AKASA
Feb 1, 2023
AKASA is the preeminent provider of generative AI solutions for the healthcare revenue cycle.









