Real ROI for Montage
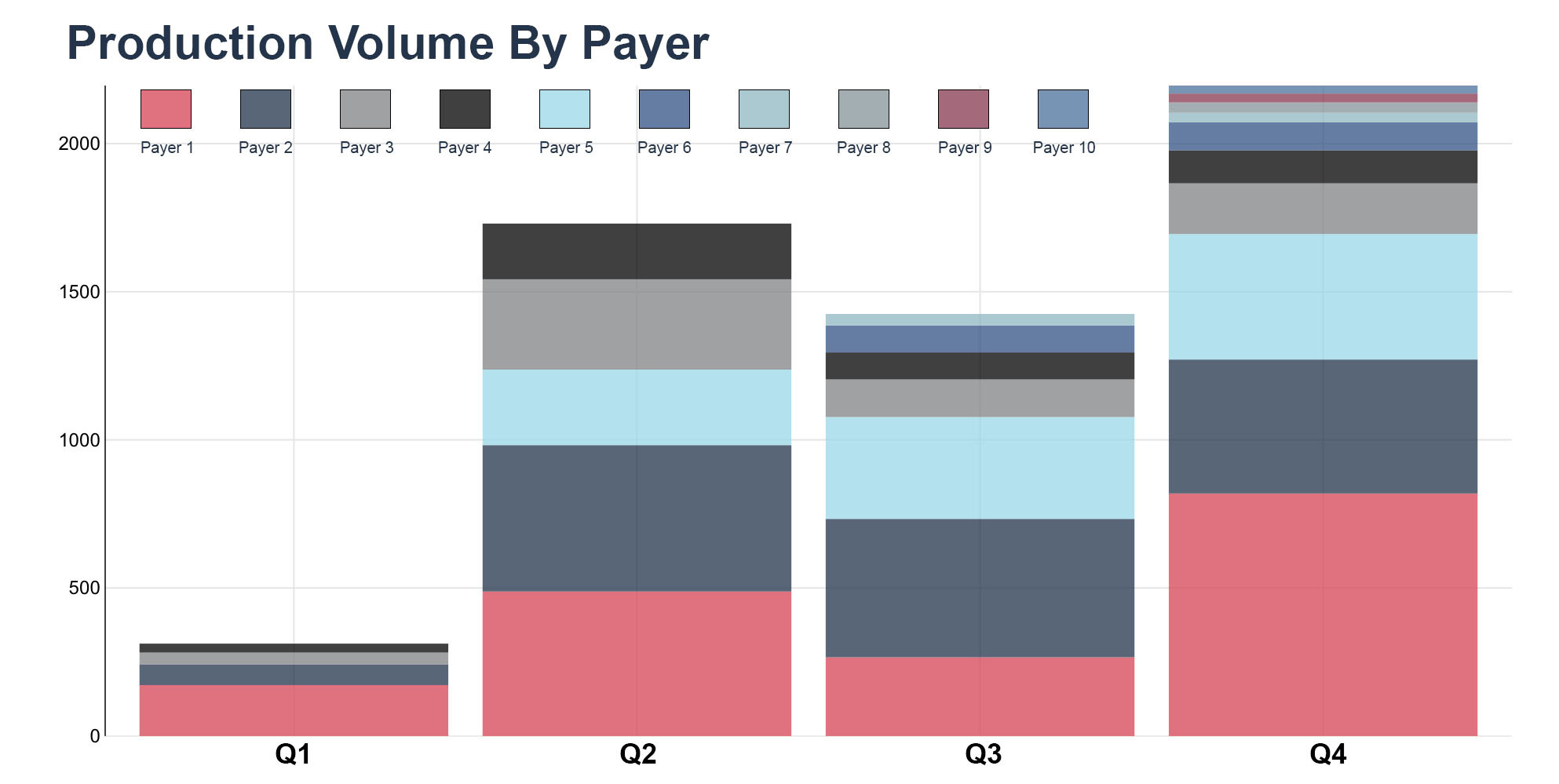
Reduced auth work queue volume 22%
See how Montage Health collaborated with AKASA to improve their prior authorization processes, create efficiency, and drive value.
See how Montage Health collaborated with AKASA to improve their prior authorization processes, create efficiency, and drive value.
Methodist Health System, a leading care provider in Nebraska, worked with AKASA to obtain timely status for outstanding claims. See how we removed 71.3% of accounts from staff queues, did the status work of nearly 14 full-time employees, and more.