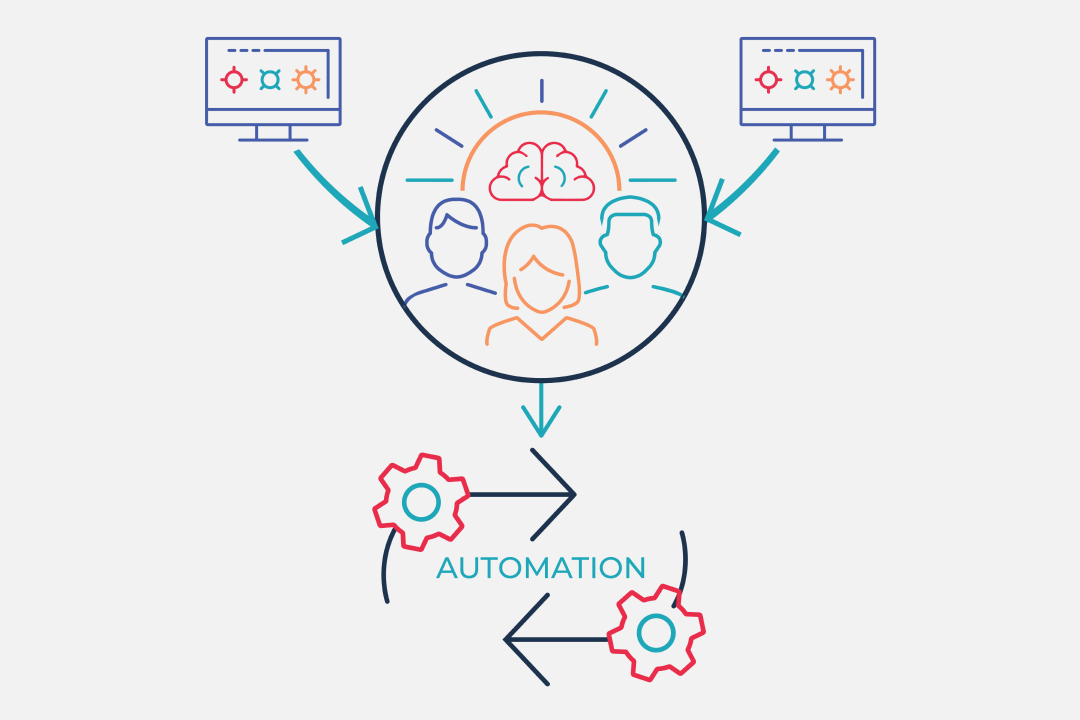
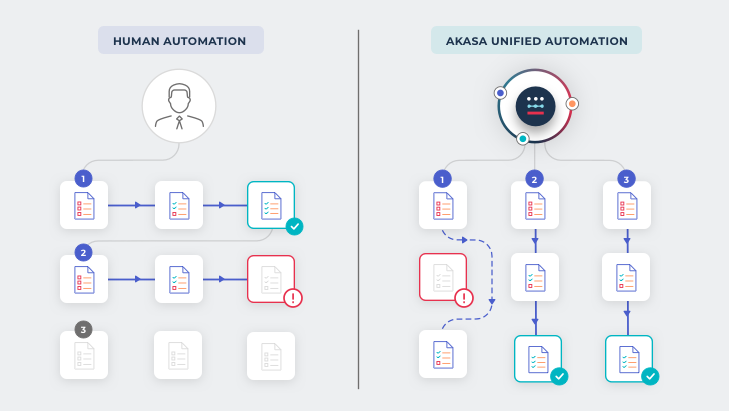
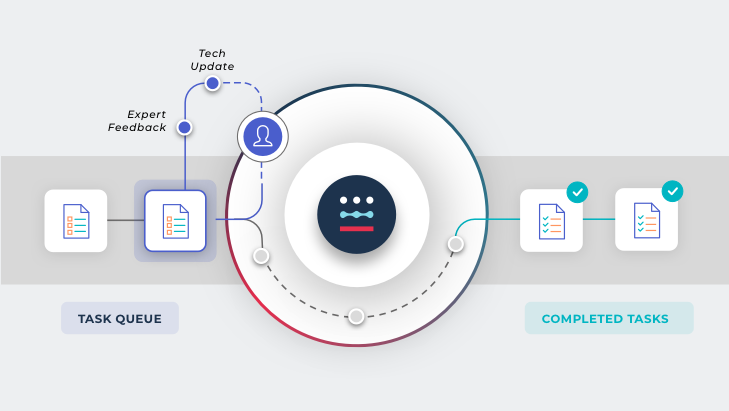
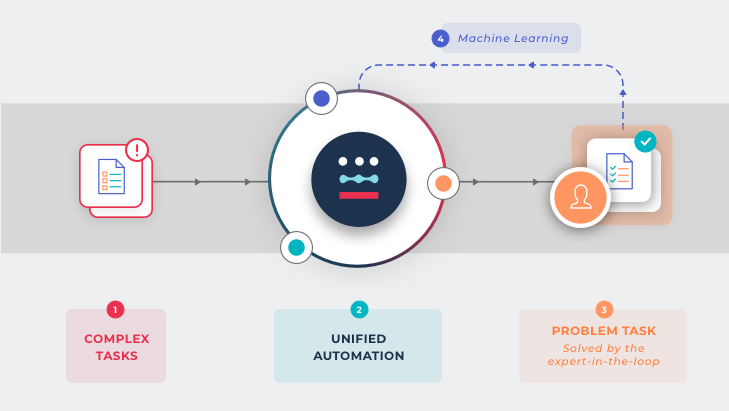
The Unified Automation process
Proprietary Software Observes
AI Performs
Revenue Cycle Expertise Ensures
The benefits of Unified Automation
- Operates remotely and on top of existing billing and EHR systems
- Eliminates the need for consultants, in-person implementations, multiple vendors, or new staff to manage processes
- Allows value to be delivered faster and on a constant basis, with almost no maintenance
290M
Number of claims and remittances Unified Automation has been trained on
We have been impressed with the AKASA team’s expertise in revenue cycle operations. They were able to deploy Unified Automation quickly, and we’ve seen the system adjust to process changes in real-time.
Jeff Francis — Vice President and CFO, Methodist Health System